DIME PROJECT

Building healthcare around the patient, not the clinic

Technical & operational considerations
A successful hospital-at-home (HaH) program requires a robust technical infrastructure and a well-designed operational framework. Both elements must work together seamlessly to deliver acute-level care safely and reliably in the home environment.
This resource outlines the foundational components of a scalable, patient-centered HaH model, highlighting key considerations for technology selection, interoperability, workforce readiness, clinical workflows, and in-home logistics. Review these best practices to help you achieve clinical excellence, operational efficiency, and long-term sustainability. Explore the interactive version below, or download the pdf version.
I. Establish your technical foundation
Building a HaH technical foundation involves more than selecting digital health technologies (DHTs). It requires a cohesive, integrated ecosystem that extends the hospital’s clinical, operational, and data capabilities safely into the home. From remote patient monitoring (RPM) and electronic health record (EHR) integration to secure telehealth and medication management, every component must work together to ensure seamless communication, timely intervention, and clinical continuity. This section outlines the technology stack, EHR integration, usability, connectivity, and security/privacy considerations essential for delivering reliable, patient-centered care in a distributed environment.
Establish an integrated system that enables hospital-level care delivery in the home, supporting monitoring, communication, coordination, and rapid response.
- Deploy remote monitoring tools to support care between in-person visits
- Use RPM technologies to track vital signs, conduct electrocardiograms (ECGs), and monitor glucose levels, falls, and pain levels.
- Leverage FDA-authorized/CE-marked tools to meet requirements for major reimbursement pathways.
- Consider emerging technologies to promote innovation in the HaH setting.
- Refer to RPM Resources Kit (CTA-2101).
- Implement a fit-for-purpose telehealth platform
- Enable video visits and remote clinical documentation for virtual care delivery.
- Refer to Best Practices and Recommendations for Telehealth Solutions (ANSI/CTA-2113).
- Enable video visits and remote clinical documentation for virtual care delivery.
- Adopt a care coordination platform designed for HaH
- Support task management, real-time communication, and care plan documentation.
- Include built-in triage and escalation capabilities with automated alerts for coordinated oversight and emergency management.
- Set up medication management systems
- Implement e-prescribing with interaction checks, track adherence, and set up alerts for missed doses. Establish seamless, bidirectional data exchange between home-based systems and hospital infrastructure to support continuity of care, provider trust, and accurate documentation.
Refer to the AWS Stel Life Case Study for an example of remote monitoring technology that enables passive vital sign tracking and supports integrated care coordination in home-based settings.
Create seamless, bidirectional data exchange between home-based systems and hospital infrastructure to support continuity of care, provider trust, and accurate documentation.
- Integrate with your existing EHR using standard protocols
- Use FHIR APIs and HL7 messaging standards to sync clinical notes, medication orders, and diagnostics.
- Refer to Guiding Principles of Practice and Transparency for Mobile Health Solutions (CTA-2073).
- Implement single sign-on (SSO) and define clear read/write permissions for all team members, including role-based, mobile access.
- Use FHIR APIs and HL7 messaging standards to sync clinical notes, medication orders, and diagnostics.
- Design for system-wide interoperability and version control
- Ensure updates to software and DHT models maintain compatibility with workflows and data formats.
- Document model governance and maintain audit trails for regulatory compliance.
- Refer to the FDA Digital Health Policy Navigator for guidance on regulation, governance, and compliance.
- Ensure patient data is captured in a format that facilitates accurate documentation and effective communication.
- Refer to Health Data: Reporting Format Best Practices (ANSI/CTA-2093).
- Anticipate enterprise integration needs
- Build infrastructure that supports large-scale deployment of DHTs and platforms within home settings and the broader hospital ecosystem.
Validate tools to empower patients and care partners through intuitive design, clear communication, and accessible education to enhance trust, engagement, and safety.
- Offer patient-facing technologies tailored for diverse needs
- Provide tablets or apps with multilingual support, low-literacy accessibility, and intuitive interfaces.
- Enable secure two-way messaging, daily check-ins, and personalized education modules for active patient engagement.
- Support shared decision-making with patients and care partners
- Involve patients and care partners in co-design efforts to ensure tools are practical and trusted.
- Include features that promote transparency, goal setting, real-time updates, and collaboration with patients and care partners.
- Ensure alignment with clinical workflows
- Coordinate human-centered design with care team input to avoid disruptions in communication, documentation, or handoffs.
- Refer to DiMe’s V3+ framework to ensure user-centricity and scalability of sensor-based digital health technologies.
- Collaborate with IT and clinical teams to ensure consistent DHT performance across platforms and alignment with provider workflows and documentation standards.
- Refer to Evidence Based Performance Criteria for Digital Therapeutics (ANSI/CTA-2109).
- Coordinate human-centered design with care team input to avoid disruptions in communication, documentation, or handoffs.
Refer to baseline evidence criteria for usability compiled in DiMe’s High-Quality Evidence for DHTs checklist.
Ensure reliable, near real-time data transmission and continuous functionality of DHTs in diverse home environments.
- Deploy DHTs that support consistent, secure data transmission
- Provide near real-time transfer of critical vitals (< 30 seconds) and DHTs with 24+ hour battery life.
- Support remote troubleshooting and maintenance for proactive resolution.
- Implement safeguards for connectivity disruptions
- Use automated alerts for out-of-range vitals or data transmission failures.
- Ensure offline functionality in mobile platforms with clear fallback protocols.
- Assess home environments prior to deployment
- Verify broadband or cellular coverage and provide equipment (e.g., Wi-Fi hotspots) as needed to support clinical reliability.
Uphold hospital-grade data protection standards across all in-home technologies to maintain trust, safeguard sensitive information, and ensure regulatory compliance.
- Establish a strong cybersecurity framework
- Enforce end-to-end encryption and multi-factor authentication (MFA) for all data access points.
- Deploy AI-driven threat detection and real-time security alerts to identify and mitigate vulnerabilities.
- Refer to Baseline Cybersecurity Standard for Devices and Device Systems (ANSI/CTA-2088-A).
- Ensure vendor and DHT compliance
- Build robust data governance and response systems
- Maintain audit trails, consent management documentation, and automated compliance reporting.
- Create and regularly update incident response plans for potential data breaches or DHT-related security threats.
Refer to baseline evidence criteria for security and privacy compiled in DiMe’s High-Quality Evidence for DHTs checklist.
II. Design & implement your operational framework
An effective HaH program depends on a well-orchestrated operational framework that replicates hospital-level care in the home setting. This includes staffing models, logistics, protocols, patient selection, measurement, and training practices tailored to the complexities of in-home care. Success hinges on clear workflows, defined roles, and strong coordination across teams and sites. In this section, you’ll find guidance on building agile infrastructure, aligning with brick-and-mortar (BAM) facilities, training care teams, and measuring outcomes to ensure safety, consistency, and scalability.
Design a workforce model that blends virtual and in-home roles to provide continuous, acute-level care in the home environment.
- Establish adaptable staffing structures
- Combine mobile care teams (registered nurses, paramedics, ancillary staff) with virtual roles in command centers or remote clinical support.
- Leverage shared resources across departments/facilities, and use per diem pools or cross-coverage arrangements, to address workforce constraints.
- Ensure credentialing, licensure, and liability compliance
- Verify licensure for clinicians practicing across state lines in virtual settings.
- Address liability coverage for in-home services and inter-facility workforce sharing.
- Explore systemwide credentialing to support flexible staffing across locations.
- Clearly define roles and responsibilities
- Identify expectations for each team member (in-home nurse, remote provider, dispatch coordinator, etc.) using standard, role-based workflows.
- Define care team structure, decision-making authority, and escalation responsibilities to ensure accountability.
- Clarify distinctions between HaH and BAM care teams, specifying their respective roles in patient assessment, history and physical (H&P) exam performance, and care planning.
- Refer to Mount Sinai’s Staffing the Hospital at Home Program guide.
Develop operational systems that support real-time care delivery, communication, and supply coordination across dispersed settings.
- Select a command and coordination model
- Select between centralized command centers, lean hubs, or distributed coordination structures, depending on the program’s scale and geography.
- Support mobile care teams
- Equip clinical teams with EHR access to document notes, log vitals, and communicate securely while in the field for in-home visits, assessments, and interventions.
- Coordinate transportation and field operations
- Provide access to reliable vehicles and scheduling systems for mobile visits.
- Establish patient transport protocols for urgent escalations, community appointments, or facility transfers.
- Streamline delivery of medications, equipment, and services
- Develop logistics systems for timely delivery of meds, oxygen, durable medical equipment (DME), lab kits, and meals.
- Enable secure, temperature-controlled deliveries with GPS tracking and escalation protocols supported by AI triage for 24/7 response.
- Establish vendor service-level agreements (SLAs) for delivery accuracy, timeframe, and quality assurance.
Build comprehensive care pathways that mirror inpatient processes and meet regulatory and quality standards in the home.
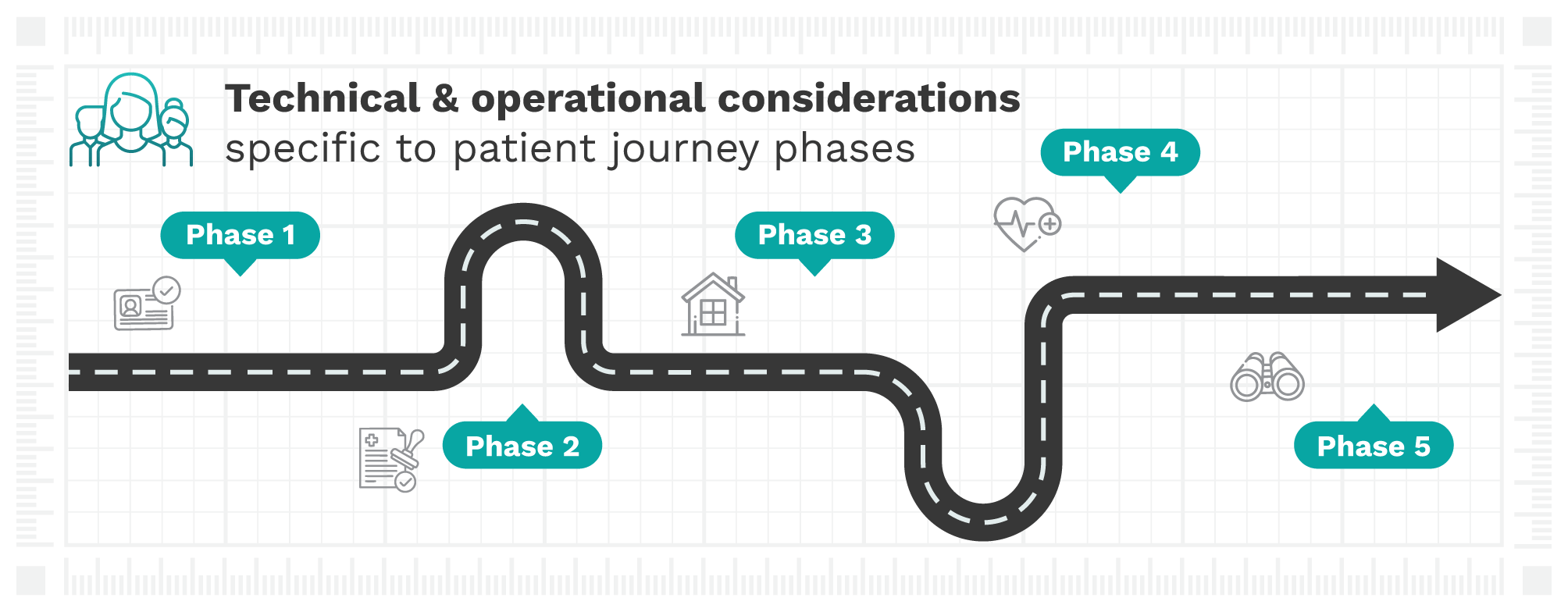
- Map home-based workflows from intake through discharge
- Define tasks within each phase of the patient journey, including triage, monitoring, escalation, and wraparound support.
- Refer to Section 1: Patient Journey Map.
- Confirm the timing, location, and responsible provider for the first in-person patient exam to determine when admission orders and care plans are written and when remote provider consultations begin.
- Define tasks within each phase of the patient journey, including triage, monitoring, escalation, and wraparound support.
- Create standardized protocols and escalation pathways
- Use evidence-based care plans for high-volume or high-risk conditions.
- Define response time expectations with ecosystem partners (e.g., logistics, DME, mobile care teams) within SLAs to coordinate efficient escalation management.
- Set clear thresholds for when to escalate care or transfer patients back to the hospital.
- Coordinate with brick-and-mortar (BAM) facilities
- Define joint admission and transfer or discharge criteria with emergency departments (EDs) and inpatient units.
- Use shared communication workflows and documentation protocols for warm handoffs.
- Recognize patient movement rate, including all transitions and planned care outside the home, as an operational complexity requiring continuous monitoring and coordination to minimize disruptions.
- Ensure documentation meets CMS Conditions of Participation (CoPs) as needed
- All clinical records must comply with hospital-level CoPs, even in the home, to participate in Medicare and Medicaid programs.
- Implement real-time charting, audit trail capture, and compliance with medical necessity and billing standards.
Select patients who are appropriate and match care intensity to their clinical and social risk factors to ensure safety and success.
- Define clear eligibility and screening criteria
- Screen for diagnosis, clinical stability, home safety, and care partner support.
- Leverage AI to enhance patient identification and eligibility determination with rules-based algorithms.
- Develop pathways for both direct admission to HaH and timely transition from inpatient care, with referrals facilitated by electronic flags and appropriate checkpoints in the admission process.
- Implement a robust risk stratification model
- Tailor RPM frequency and visit cadence to patient acuity.
- Reassess risk regularly and adjust care plans and escalation protocols as needed.
- Incorporate social determinants of health (SDOH), area deprivation index (ADI) and care partner insights
- Use standardized screening tools from CMS or PRAPARE to identify and action non-clinical risk factors, including SDOH, that may impact patient safety or success at home.
- Evaluate ADI to inform risk stratification and program expansion to address the unmet needs of additional patients (e.g., meals services, caregiver support).
- Refer to the ADI Neighborhood Atlas.
Use data to drive continuous improvement, track return on investment (ROI), and support reimbursement conversations. Refer to Section 3: Program evaluation & reimbursement pathways.
- Align measurement strategies with business priorities
- Compare HaH to traditional inpatient care by measuring program performance, ROI, and cost.
- Drive payor adoption and promote value-based care integration by demonstrating HaH’s value proposition and alignment with other home-based care models (e.g., SNF-, hospice-, and ED-at-home).
- Monitor key measures to evaluate program value and impact
- Track clinical, quality, & safety outcomes, access, equity, & experience, cost & resource utilization, and operational performance & efficiency.
- Use dashboards and conduct weekly reviews to spot trends, resolve delays, and translate impact into value propositions for key stakeholders.
- Build systems for feedback and iteration
- Engage frontline teams in identifying process gaps and co-developing data-driven solutions.
- Use root cause analysis for adverse events and escalations to refine clinical workflows and training.
Prepare all team members, including care partners, to deliver safe, high-quality care in the home.
- Implement comprehensive training programs
- Cover clinical and social assessments, in-home care, DHT usage, documentation workflows, and safety protocols in training programs for staff and care partners.
- Use simulation-based education for high-risk scenarios like equipment failure or patient deterioration.
- Establish and train staff on service level agreements (SLAs)
- Collaborate with home health agencies, diagnostics vendors, logistics partners, and meal providers to guarantee consistent quality.
- Enhance cultural competency and communication
- Provide training focused on respectful, effective communication strategies for diverse patient populations and perspectives.
- Promote ongoing education and skill developmen
- Set up continuous professional development opportunities for staff focused on emerging technologies, regulations, and evidence-based best practices.
- Explore continuing education resources for your team, such as AMA Ed Hub.