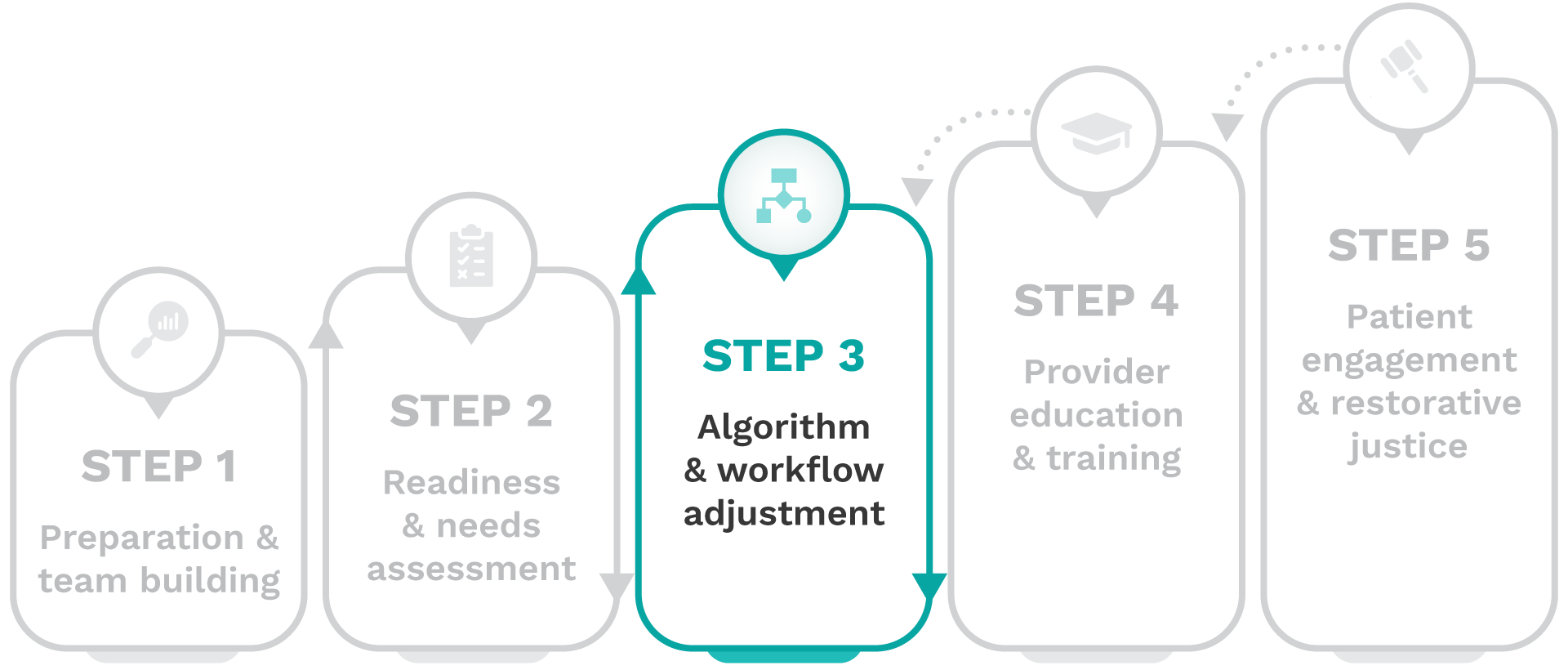
Removing harmful race-based clinical algorithms: A toolkit

Step 3-Algorithm & workflow adjustment
Step 3 is where you will develop and execute a focused work plan to remove each harmful clinical algorithm one at a time. You will replace your identified algorithms with an evidence-based alternative, and refine workflows to support sustainable, equitable practices.
Important stakeholders
Key stakeholders involved in the de-implementation process of the specific algorithm, including executive and health equity leadership, clinical and non-clinical staff, IT and data teams, and patient advisory groups, who collaborate to effectively adjust workflows related to the algorithm.
Complete these activities
To achieve this goal, complete the following activities:
1. Identify race-based algorithms
Investigate the institution’s use of race-based clinical algorithms to identify areas of bias in care delivery and resource allocation decision-making.
The toolkit places an emphasis on the clinical algorithms from the first iteration of CERCA focused on kidney function (eGFR), pulmonary function (PFT), and pregnancy-related tools (VBAC). However, there are many more examples of decision-making in healthcare that include a race variable. Review these more detailed repositories to identify race-based clinical algorithms that may be used at your institution, considering the unique needs of your patient population.
2. Select a harmful algorithm
Select a harmful race-based algorithm, research its history and rationale for including race, and contextualize its impact on patient care, including clinical patient outcome measures recommended in the toolkit.
Lessons from CERCA and real-world clinical practice can help guide the selection of a harmful race-based clinical algorithm for de-implementation at your institution.
- Estimated glomerular filtration rate (eGFR): All institutions that chose eGFR successfully de-implemented the race-adjusted algorithm, with some making the change even before joining the coalition. This decision was supported by the strong endorsement of the race-neutral alternative equation by the NKF-ASN task force.
- Pulmonary function testing (PFT): Due to the costs of hardware and software updates, collective efforts to secure grant funding delayed PFT algorithm de-implementation. Of the 8 institutions that selected PFT, 5 were still in the planning stages as of 2024.
- Vaginal birth after cesarean section (VBAC) calculator: Upon further review, CERCA institutions focusing on VBAC reported minimal use of the VBAC calculator itself. However, they recognized that race often influenced clinical decision-making around counseling and labor for vaginal births after prior cesareans. In response, CERCA’s VBAC subcommittee emphasized the importance of race-conscious, shared decision-making.
Researching the history and rationale for the use of race in algorithms like eGFR, PFT, and VBAC—and assessing their impact on patient care—can be complex and time-intensive. To support this process, review these three research spotlights, detailing the background, findings, and lessons learned from the literature for each algorithm.
- Updating the eGFR equation for kidney function: View case study
- Historical roots of race-based pulmonary function testing (PFT): View case study
- Historical roots of race inclusion in the vaginal birth after cesarean section (VBAC) calculator: View case study
3. Engage a provider champion
Identify and engage a provider champion with direct patient touchpoints and clinical expertise to guide the de-implementation of the harmful race-based clinical algorithm.
4. Map the algorithm’s workflow
Map the complete scope of the harmful race-based algorithm’s use, identifying where it appears within internal systems including workflows, educational materials, and patient-facing resources.
5. Develop and execute fundraising
Develop and execute a targeted fundraising strategy to secure financial resources for de-implementation efforts for the selected algorithm.
Securing funding for new hardware and software in healthcare requires a strategic, data-driven approach. Start by:
- Collaborating with key stakeholders to document the impact of outdated systems in your institution and across your system.
- Tracking concerns, such as inaccuracy, workflow inefficiency, or inequitable patient outcomes.
- Developing a clear, compelling case to outline the problem, necessary updates, and benefits to your patients and organization.
For example, with spirometry for pulmonary function tests (PFTs), outdated equipment may not support updated software with race-neutral equations, reinforcing disparities in pulmonology and making a strong case for investment in new hardware.
Engage leadership with evidence-based messaging, explore multiple funding avenues, and stay persistent—funding decisions often rely on both a strong justification and the right timing.
- Securing hardware for race-neutral PFT at SBH Health System: View case study
6. Remove the harmful algorithm
Remove the selected algorithm from all workflows, educational materials, and patient-facing resources, ensuring the de-implemented algorithm can no longer be used under any circumstances.
When updating race-based clinical algorithms like eGFR, it’s essential to remove outdated equations from lab reporting, integrate the revised formula into the EHR, and ensure all clinical workflows reflect the change. Additionally, monitor external lab partners and referral networks to confirm alignment, preventing outdated algorithms from re-entering patient care decision-making.
7. Implement an alternative
Implement an evidence-based alternative or more nuanced shared decision-making approach when there is evidence of harm but insufficient research for an alternative tool.
VBAC calculators are typically accessed online at the clinician’s discretion and function as decision-support tools rather than EHR-embedded algorithms. Removing race from these tools is crucial, but more importantly, VBAC decisions should be guided by shared decision-making, ensuring that patient values, preferences, and individualized risk assessments take priority over a calculator’s outputs. Even calculators that do not include race may introduce bias through other problematic inputs, such as BMI and chronic hypertension, reinforcing the need for personalized care and clinician counseling rather than sole reliance on predictive models.
8. Monitor workflow adjustments
Conduct ongoing monitoring of workflow adjustments and make iterative refinements to ensure it aligns with evidence-based practice, institutional priorities, and use by external partners.
9. Track patient outcomes
Track the clinical patient outcome measures selected from the toolkit to assess the impact of de-implementation and ensure no new harm is introduced.
Below are priority outcome measures for kidney function, pulmonary function, and vaginal birth after cesarean section based on our research:
- Estimated glomerular filtration rate (eGFR):
- Referral or current care provided by nephrologist
- Referral or waitlist status for kidney transplantation
- CKD stage reclassification
- Utilization of medications to slow CKD progression
- Prevalence of CKD by stage
- Pulmonary function testing (PFT):
- Diagnosis of lung disease
- Referral to pulmonologists
- Prevalence of obstructive & restrictive pulmonary disease, overall & by severity
- Prescription of medications for lung diseases as recommended by COPD & asthma guidelines
- Reclassification of lung disease severity
- Vaginal birth after cesarean section (VBAC):
- VBAC rates
- Trial of labor after cesarean section (TOLAC) rates
- Postpartum complication rates
- Vaginal birth rate
- Primary and repeat cesarean rates
When tracking patient outcomes, some changes may initially appear negative due to shifts in data collection methods, pre-existing biases, or other factors beyond race and ethnicity. Apply a nuanced approach that accounts for potential confounders to ensure an accurate assessment of both the long-term benefits and challenges of de-implementation. Additionally, consider that while de-implementation can lead to positive downstream effects, unintended consequences may also emerge, underscoring the importance of continuous monitoring.
10. Involve providers
Involve providers throughout the de-implementation process to gather feedback on workflow adjustments and ensure alignment with race-conscious care practices.
11. Gather patient feedback
Collect patient advisory feedback on preferences for how care should be delivered, ensuring that the de-implementation process reflects patient needs and values.
Clinical Outcome Measures: eGFR
PRIORITIZED TOP 5: Primary
- Referral or current care provided by nephrologist
- Referral or waitlist status for kidney transplantation
- CKD stage reclassification Utilization of
- medications to slow CKD progression
- Prevalence of CKD by stage
Clinical Outcome Measures: PFT
PRIORITIZED TOP 5: Primary
- Diagnosis of lung disease
- Referral to pulmonologists
- Prevalence of obstructive & restrictive pulmonary disease, overall & by severity
- Prescription of medications for lung diseases as recommended by COPD & asthma guidelines
- Reclassification of lung disease severity
Clinical Outcome Measures: VBAC
PRIORITIZED TOP 5: Primary
- VBAC rates
- TOLAC rates
- Postpartum complication rates
- Vaginal birth rate
- Primary and repeat cesarean rates
Track your progress
Use the Dynamic Scorecard for each algorithm to track milestones and key performance indicators (KPIs) suited to your institution’s pursuit of harmful race-based clinical algorithm de-implementation.

Next steps
Once you have completed these activities, the selected harmful race-based algorithm will be fully removed, and an effective, equitable alternative will be integrated into your workflows and practices to promote race-conscious patient care and sustainable institutional change.



