DIME PROJECT

Implementing AI in Healthcare
Unlock cumulative AI value in healthcare workflows
Many systems overlook the power of incremental gains in high-volume, high-frequency workflows where AI thrives. By focusing on “stackable wins”, you can drive cumulative ROI while building institutional confidence and capability over time.
Look for AI tools that embed seamlessly into these workflows and free up frontline capacity. Think patient registration, prior authorization checks, routine medication refills, or discharge instructions. These repetitive, rules-based tasks are ripe for automation, and even a small time savings at the task level can “stack” into recovered staff time, reduced delays, and better throughput across the enterprise.
Common characteristics of tasks ripe for AI automation
High frequency (thousands of times per day)
Standardized or semi-structured processes
Low clinical ambiguity
Clear handoffs between systems or staff roles
Stackable Wins Pyramid
The interactive graphic below illustrates how cumulative efficiencies compound over time. Use it to prioritize implementation opportunities based on complexity, risk, and volume to de-risk early deployment and accelerate system-wide impact.
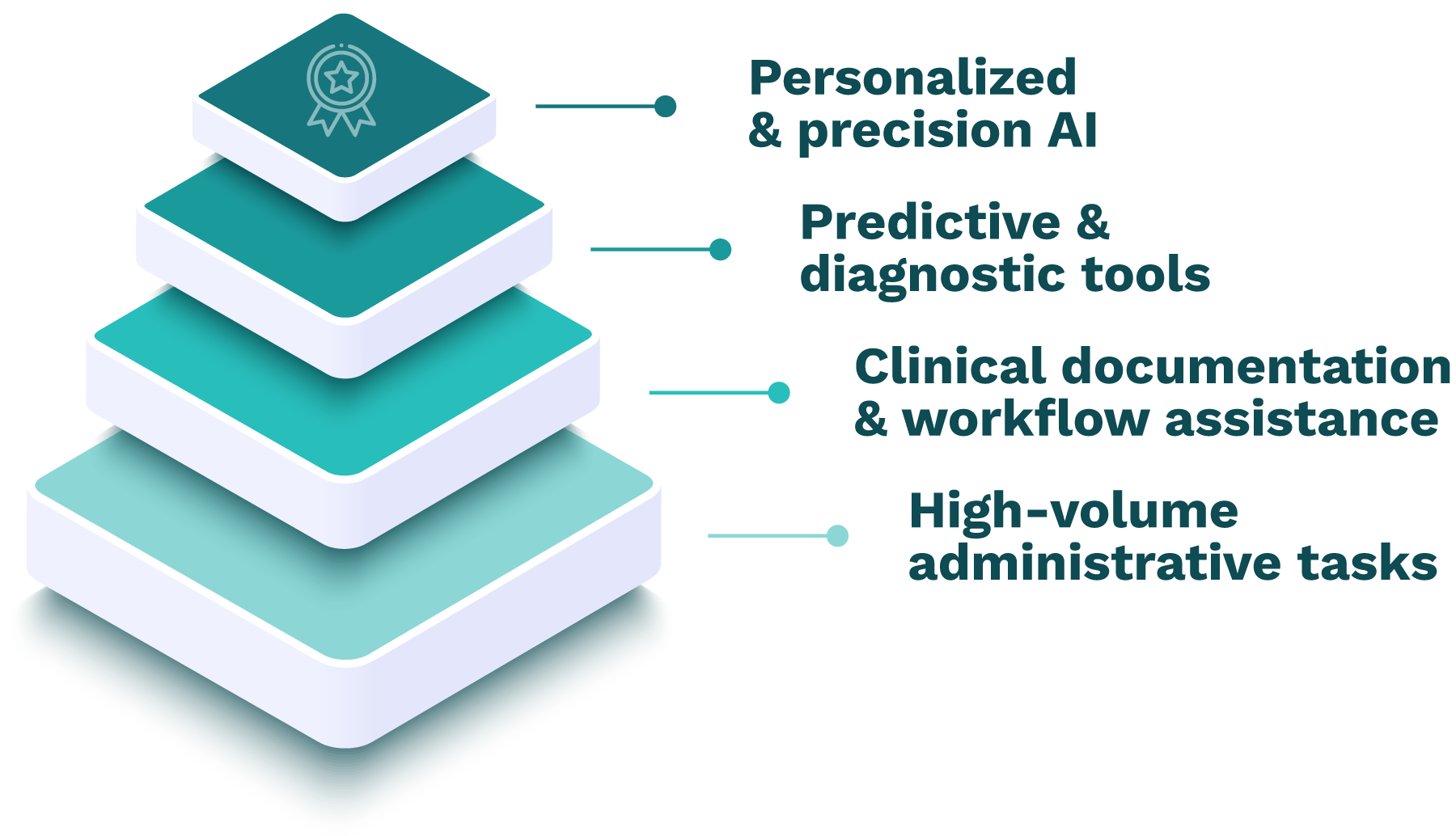
Personalized & precision AI (Few/week)
Use case: Pharmacogenomics, individualized pathways
AI role: Multi-modal data fusion for treatment optimization
Workflow integration: Embedded in clinical decision-making moments
Value: Tailored care, reduced waste, future-state transformation
Note: High complexity, low immediate ROI. Requires significant workflow adaptation.
Predictive & diagnostic tools (Dozens/day)
Use case: Readmission risk scoring, sepsis prediction, radiology triage
AI role: Predictive modeling based on health record or imaging data
Workflow integration: Alert delivery at natural decision points
Value: Proactive care, safety, resource optimization
Note: High governance burden. Must prove real-world value without workflow disruption.
Clinical documentation & workflow assistance (Hundreds/day)
Use case: Ambient scribing, discharge summary drafting, task routing
AI role: Summarization, predictive automation
Workflow integration: Background processing during natural clinical interactions
Value: Clinician satisfaction, revenue lift, burnout reduction
Note: Success depends entirely on preserving natural clinical conversation flows.
High-volume administrative tasks (Thousands/day)
Use case: Patient registration, insurance verification, appointment reminders, prior authorization
AI role: Automate structured processes
Workflow integration: Behind-the-scenes automation of routine processes
Value: Staff time recovery, fewer errors, faster throughput
Note: High reward, low risk.
Ideal entry point—minimal workflow disruption.
Where can AI deliver impact?
Not all AI domains integrate equally well with existing healthcare workflows. Use this overview to understand where AI is likely to perform reliably within current work patterns and where it may require significant workflow adaptation or introduce higher implementation risk.
Mature solutions should integrate smoothly; emerging tools require careful workflow redesign and piloting. Select vendors not just for features, but for their proven ability to integrate seamlessly, support workflow preservation, and evolve with your system’s natural work patterns.
Defining maturity status
Widely deployed: Solutions are validated, regulated (often under FDA oversight), and used at scale.
Scaling: Demonstrated efficacy and ROI in pilots or early deployments.
Emerging: Still in early testing or concept phase. Requires more vetting and piloting.
|
Status |
Use cases |
Enablers |
Barriers |
Business value |
|
Widely deployed |
Radiology triage, image interpretation, incidental findings detection |
✅ FDA-cleared tools ✅ Mature data & infrastructure |
❌ Commoditizing vendor space ❌ Integration costs still high |
Faster, more accurate diagnoses Workload reduction Precision Increased throughput |
|
Status |
Use cases |
Enablers |
Barriers |
Business value |
|
Scaling |
Sepsis prediction, readmission risk, order recommendations |
✅ Regulatory clarity emerging ✅ Strong clinical demand |
❌ Alert fatigue risks ❌ Governance and validation burdens |
Augmented decision-making Improved outcomes Efficiency Cost containment |
|
Status |
Use cases |
Enablers |
Barriers |
Business value |
|
Scaling |
Sepsis prediction, readmission risk, order recommendations |
✅ Regulatory clarity emerging ✅ Strong clinical demand |
❌ Alert fatigue risks ❌ Governance and validation burdens |
Augmented decision-making Improved outcomes Efficiency Cost containment |
|
Status |
Use cases |
Enablers |
Barriers |
Business value |
|
Scaling |
Chronic disease tracking, post-op monitoring, vitals from wearables |
✅ RPM codes exist ✅ Consumer digital health technology adoption |
❌ Data quality variability ❌ Integration with clinical systems |
Early intervention Cost reduction Resource optimization Patient retention |
|
Status |
Use cases |
Enablers |
Barriers |
Business value |
|
Scaling |
AI chatbots, patient FAQs, education, and translation tools |
✅ High patient demand ✅ Fast LLM evolution |
❌ Risk of misinformation ❌ Cultural and accessibility gaps |
24/7 support Staff efficiency Consistent and multilingual outreach Increased retention |
|
Status |
Use cases |
Enablers |
Barriers |
Business value |
|
Emerging |
Precision oncology, pharmacogenomics, pathway optimization |
✅ Scientific momentum ✅ Academic/industry partnerships |
❌ Data standardization gaps ❌ Payer & clinical adoption slow |
Tailored treatments Timely care Reduced waste Better outcomes |
Next steps
Now that you’ve identified where AI can deliver the greatest impact, the next step is deciding how to source your solution. Explore whether building, buying, or partnering best aligns with your workflows, capabilities, and long-term strategy.



