ACCESS Granted: A New Era of Digital Care for Medicare Beneficiaries
 In 2020, our team at the Digital Medicine Society (DiMe) launched the Virtual-First Care (V1C) Coalition. I was concerned that V1C was becoming overfit for direct-to-consumer models and:
In 2020, our team at the Digital Medicine Society (DiMe) launched the Virtual-First Care (V1C) Coalition. I was concerned that V1C was becoming overfit for direct-to-consumer models and:
- The individuals who would benefit most from complete care solutions, whenever and wherever they needed it, would miss out, and
- The enormous potential of V1C to address the maldistribution of clinicians and the persistent fallacy that chronic, complex conditions can be treated through episodic visits alone would be squandered.
Through our work with the V1C Coalition and the extraordinary efforts of those committed to expanding access to optimized care, V1C is now part of the rich and complex tapestry of healthcare delivery. For commercially insured patients, access signals are strong. Care coordination between V1C and traditional providers is the norm. And while we have (thankfully) dropped the absurd “omnichannel” branding, I think few in healthcare would argue against hybrid care being the future.
Yet because Medicare payment barriers created a regulatory moat, millions of Original Medicare beneficiaries have remained shut out from the benefits of modern care.
You cannot blow up the castle
One of the greatest challenges in healthcare innovation is the tug-of-war between those who want to blow up the existing system and those who cling to the status quo. At best, this tension yields incremental improvements.
The reality is that we cannot burn the existing system to the ground and hope a phoenix rises from the ashes. Healthcare is 20% of GDP; behave yourselves. Loud disruptors often disappear once the fire turns to rubble. Also, and I say this personally as someone whose life depends on this flawed system continuing to function while I battle a complex cancer diagnosis, please do not burn it down with the people you love still inside.
The drawbridge lowers…
And this is why the CMS’s ACCESS (Advancing Chronic Care with Effective, Scaleable Solutions) Model is so good. It is an elegant and pragmatic solution that lowers the drawbridge, providing an on-ramp for innovative solution providers to cross the moat and finally reach the 33+ million people who, to date, have been shut out of modern care advances.
ACCESS increases options for patients. It enables traditional providers to practice at the top of their license without untenable risk or administrative burden. And it opens the castle to a competitive market that encourages digital innovators to earn trust and drive outcomes.
For the first time, Original Medicare beneficiaries can choose high-touch, digitally enabled solutions as a routine, reimbursed part of their care, not a luxury only others can access.
Better care than a 15-minute box
I have a friend who is a primary care clinician. His biggest frustration – one which ultimately drove him to create his own data-driven V1C practice – was being forced into a rigid 15-minute template no matter the needs of the person in front of him.
Digital strategies can finally break that model.
They allow primary care providers to handle what only they can solve, and enable trusted digital health partners to deliver continuous, “between-visit” support for what they specialize in. This is what care load balancing and practice optimization looks like in practice. And now, finally, it can exist for those who rely on Original Medicare.
Priorities are clear, and the goals are consistent
Aligned with administration priorities, the ACCESS Model is focused on digitally supported chronic disease management in four key domains:
- Early cardio-kidney-metabolic conditions (hypertension, dyslipidemia, obesity/overweight, prediabetes)
- Cardio-kidney-metabolic conditions (diabetes, CKD 3a/3b, atherosclerotic cardiovascular disease)
- Musculoskeletal conditions (chronic pain)
- Behavioral health conditions (depression and anxiety)
It preserves clinician-guided care while dramatically expanding patient choice and flexibility. Which is exactly what digital technology should do.
And in exciting news from today’s event, FDA announced a new pilot program called TEMPO (Technology Enabled Meaningful Patient Outcomes). Through TEMPO, device manufacturers can request that FDA exercise enforcement discretion, including around certain premarket requirements, when their technology is deployed to ACCESS participants to improve patient outcomes as part of ACCESS-covered care. This is a major signal of regulatory alignment across agencies: CMS is lowering the drawbridge and FDA is clearing the path so effective technology can reach patients faster.
This momentum further underscores the importance of the work we have been leading with industry and regulators to advance high-quality digital measurement and outcome-based innovation. ACCESS is also deeply aligned with our Healthcare 2030 vision at DiMe:
- It puts prevention at the center of the model
- It’s seeking system-wide impact through AI-enabled precision approaches
- Payments are outcomes aligned
- Sustainability through access to solutions that can be scaled quickly and affordability is the goal
It is energizing to see industry and government lining up on what success looks like in the digital era.
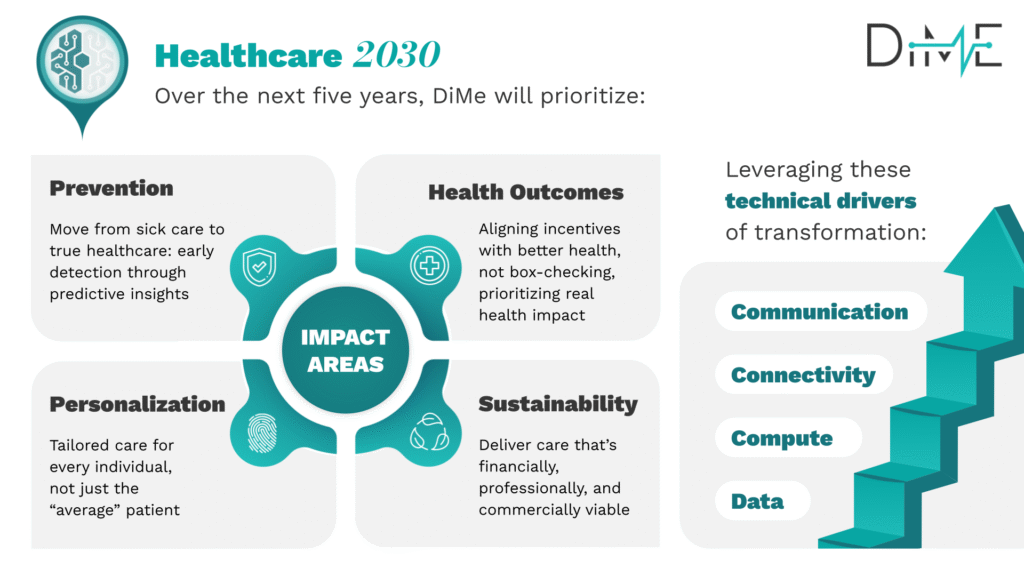
Healthcare 2030 is DiMe’s blueprint to transform US healthcare in the digital era
What it takes to keep the bridge open
The success of ACCESS will depend on three critical components:
1. Clinical outcomes must be appropriately defined
Risk-adjusted outcomes are absolutely the right move. But selecting the measures that matter will not be easy. A1c is a lazy default in diabetes. And no one should tie revenue risk in mental healthcare to PHQ-9 scores alone (hence, our work on a core digital measures set for common mental health disorders.)
2. Traditional providers must be set up to succeed in co-management
The new co-management payment recognizes their work in reviewing updates and coordinating care. Excellent. But co-management is not yet a core competency across traditional providers, and operational integration with digital solution providers is non-trivial.
3. The marketplace must function as a trusted, competitive environment
To support solution providers and referring clinicians alike, CMS will launch the ACCESS Tools Directory, an informational marketplace surfacing digital tools that support participation. Over time, clinical outcomes data used for reimbursement will be reported in the Directory, driving real, performance-based competition.
But outcomes are lagging indicators. And with more than 300,000 digital health products in the U.S., we must help people identify those that are safe, accessible, interoperable, and evidence-based.
That’s why we built the DiMe Seal, a designation that helps digital innovators differentiate their solutions based on trustworthiness, reduces provider risk in referring solutions, and allows patients to find products worthy of their confidence. We need mechanisms like this to ensure the moat is crossed safely, not recklessly.
The ripple effect: Draining the moat
In our DiMe community, leading digital solution providers want to be evaluated on performance. They have shown this courage and determination from the start and they have the data to back it up. But many are currently stuck in “Frankensteined” contracts in commercial markets requiring both outcomes and process metrics that often simply don’t align.
ACCESS offers a way to break that cycle.
It solves the immediate access problem for Medicare beneficiaries and demonstrates a scalable model for:
- Outcome-based reimbursement without endless checkboxes
- Trusted partnerships between digital and traditional providers
- A competitive market that drives clinical and financial value
If we do this right, ACCESS will not just lower the drawbridge; it will drain the regulatory and payment moat. Modern care will flow freely where it is needed most.
There is a tremendous amount of work ahead before the first pilot launches in July 2026, but the jobs to be done are clear. And the potential for ACCESS to truly transform how we care for people in the digital era is enormous.



