
Core Competency:
Clinical & Operational
Integration
Use this core competency to identify top-tier practices for integrating operational and clinical components for a seamless patient experience across care settings.
V1C providers and purchasers will discover the importance of comprehensive patient care by leveraging data analytics, optimizing clinical workflows, and fostering collaborations to facilitate care transitions within and beyond V1C.
The characteristics of exceptional V1C entities focus on the ability to connect the dots —operationally and clinically— for patients and partners across a patient journey and between providers and care settings.
They consider patient care a holistic journey rather than a transaction and invest intentionally in data analytics and interoperability, clinical workflows and wrap-around services, and collaborations that position them.
Maturity: Emerging
This new care modality must be integrated, clinically and operationally, into the existing healthcare system to recognize its full potential and add value to patients, providers, and payors, improving the overall experience of health outcomes and the economic sustainability of healthcare. V1Cs must demonstrate that they work well within a system of care that spans an entire patient journey.
High-quality V1C providers are proactive in their approach. They invest strategically in workflows, data systems, and partnerships that are designed to minimize friction during patient transitions into, between, and out of V1C.
Seamless care transitions:
- Occur in clinically relevant timeframes
- Enable the exchange of appropriate information between the right parties
- Make efficient use of health resources, including services and clinical workforce, avoiding duplication of services
- Minimize inconvenience and disruption to patients
- Produce optimal patient outcomes
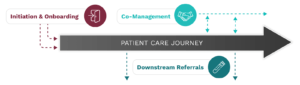
Initiation and onboarding
Intake processes should leverage a fit-for-purpose tech stack to integrate historical clinical records to verify insurance eligibility and cost-sharing and document informal care partners, patient preferences, and social determinants of health that may impact care.
Co-management
Clinical integration is the process and structures that enable provider collaboration to advance shared quality and efficiency goals at the patient and population levels. It requires a holistic and collaborative approach to patient care anchored to patient-centered primary care. Excellent V1C entities design their platforms and workflows with industry-standard data interoperability, evidence-based clinical protocols, and an outcomes-focused payment pathway.
Downstream referrals
V1C is not “virtual-only” care. Downstream referral care transitions involve services needed for a V1C to deliver care and can represent transactional, short-term services essential to completing care plans.
- Delivering a seamless patient onboarding process, including education and technology support and intake processes that streamline insurance eligibility and coverage, health record integration, medication reconciliation, and care partner coordination.
- The ability to navigate patients to downstream services, including seamless referral processes, timely and convenient scheduling, and limited out-of-pocket patient costs.
- Enabled clinical integration with other providers such as standardized bi-directional communication between clinical care teams to support quick and effective clinical decision-making.
- Operational integration with other platforms to share data that support reimbursement or quality initiatives such as HEDIS.
Other related resources:
- A Tech Stack for Effective V1C Care Transitions
- Engaging Informal Care Partners for Optimal V1C Care Transitions
- Engaging Key Partners for Effective V1C Care Transitions
- Guide to Effective Virtual-First Care (V1C) Care Transitions
- V1C Care Transitions Toolkit Resources
- Necessary Conditions for Effective V1C Care Transitions
- Quickstart Guide to Partnerships between V1C Providers and Accountable Care Organizations (ACOs)
- Quickstart Guide to Partnerships between V1C Providers and Employers
- Quickstart Guide to Partnerships between V1C Providers and Health Insurance Providers (Payors)
- Conceptualizing a Data Infrastructure for the Capture, Use, and Sharing of Patient-Generated Health Data in Care Delivery and Research through 2024
Other related case studies:
- Biofourmis: Coordinating virtual specialty care for polychronic patients
- Byteflies: Digital medicine as an enabler of effective V1C care transitions
- CareHive: Navigating patients across the continuum of care transitions
- Freespira: Virtual care partnership provides mental health care for managed Medicaid members
- Heartbeat Health: Leveraging in-home care providers to address the “last mile of care”
- Heartbeat Health: V1C partnering with ACOs for effective care transitions
- Oshi Health: Achieving whole-person care
- Thirty Madison: Seamless downstream referrals advance access to HIV prevention
- Wellinks: Integrating high-value V1C solutions for chronic disease management
Stakeholder perspectives on clinical and operational integration
-

Patients value providers who consider their medical history to understand their holistic health status and trust that their care teams are coordinated, regardless of location.
-

Providers value V1C solutions that cover the breadth of services required to treat the ‘whole person.’ Operational and clinical integration means improved member experience across the care journey and, where needed, coordination between providers that reduces duplication of services, delays, and costs.
-

Health systems & providers seek complementary V1C partnerships that effectively augment their services. Clinical integration powered by data interoperability, two-way sharing, and formal and informal partnerships enables health systems to retain patients while maintaining or improving safety, quality, timeliness of care, and satisfaction for both their providers and patients.
-

Employers value providers who deliver best-in-class customer services, are adept at attracting and retaining eligible members, and are positioned to help navigate patients to covered benefits and services outside of their practice.
-

Investors expect stage V1C providers to demonstrate how they logically fit into the more extensive health system and demonstrate the potential to scale beyond niche markets into the employer, health system, and insurance networks.
What does high quality, trustworthy V1C look like? Explore the Core Competencies framework to discover what good V1C looks like and how to get there.
Trustworthy digital experience
Deliver an ethical, equitable, and safe digital experience



