Navigating the Reimbursement Landscape in the Digital Health Era
IMPACT’s Newest Toolkit for Success
The digital health era has changed how patients interact with the healthcare system by making preventive services, specialty care, and chronic disease management more accessible than ever. As the industry continues to evolve and mature, understanding and effectively navigating the healthcare coding landscape is crucial for sustainability.
Virtual first care (V1C) is medical care for individuals or a community accessed through digital interactions where possible, guided by a clinician, and integrated into a person’s everyday life.
This innovative modality of care encourages new ways of thinking about value-based reimbursement as it takes a holistic, team-based approach to care delivery. Yet, fee-for-service reimbursement structures remain predominant despite the unique considerations for V1C delivery models.
IMPACT, a DiMe and ATA initiative, recently released the Payment & Coding Toolkit to empower providers with industry-vetted best practices for effective reimbursement strategies within the current coding landscape.
Understanding CPT codes and the current landscape
The fee-for-service model relies upon effective coding practices to translate medical diagnoses and rendered services into standardized codes on a healthcare claim, typically using the Current Procedural Terminology (CPT) developed by the American Medical Association.
Accurate coding ensures appropriate reimbursement, helping healthcare providers maintain cash flow and continue delivering quality care. Standardized coding practices also allow for more efficient processing of insurance claims, reducing delays and costly administrative errors.
Furthermore, these guidelines are critical to generating valuable healthcare data that informs quality standards, reimbursement decisions, and outcomes research. However, the landscape is complex and continually evolving with frequent updates, regulatory changes, and the introduction of new codes.
Additionally, traditional coding and reimbursement guidelines were designed for in-person visits conducted by Qualified Health Professionals (QHPs), creating gaps and misalignment with V1C delivery models and making it difficult for V1C providers to identify the best or most appropriate coding practices for reimbursement.
Introducing the IMPACT Payment and Coding Toolkit
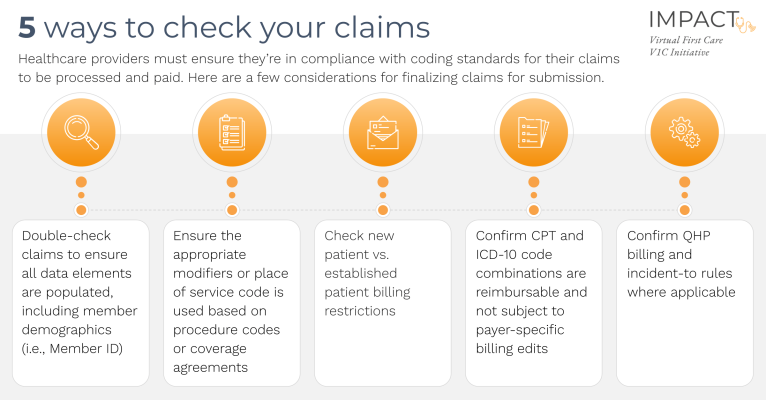
While establishing a contract is the critical first step to getting reimbursed for virtual care, healthcare providers must ensure they comply with both coding standards and contractual obligations for their claims to be processed and paid.
Recognizing the need for a comprehensive resource tailored to the unique challenges faced by V1C organizations, IMPACT developed the Payment and Coding Toolkit.
These free resources were designed to highlight avenues that are available for reimbursement within the existing fee-for-service framework and serve as a strategic guide for understanding and applying coding guidelines and industry best practices.
This toolkit gives V1C providers a quick, efficient, and reliable set of resources to better understand the complexities of healthcare coding and easily identify applicable strategies regardless of their clinical focus. It includes:
- An overview of the basics of payment and coding
- A checklist and step-by-step guide for performing essential quality checks before submitting claims for payment
- A comprehensive library of approved procedure codes, modifiers, and place of service codes for common V1C components
- Case examples of real-life best practices from industry leaders
Used broadly across the field, the toolkit will advance the use of V1C to provide medical care through digital interactions for everyone.
Highlighting best practices from industry leaders
In addition to resources designed to inform and guide users through the complexities of billing and coding, the toolkit includes case examples of proven best practices from leading V1C providers.
In partnership with Omada Health and Dreem, these payment vignettes demonstrate the real-life application of successful coding practices and provide users with tangible examples of codes for common components of care delivery models.
Dreem, recently acquired by Beacon Biosginals, established the first virtual sleep clinic, using digital technology to provide consults, diagnoses, and treatments for patients from the comfort of their own homes. Dreem’s CEO and Co-Founder, Quentin Soulet de Brugière, expressed that understanding the current coding landscape was critical to their success.
“I’ve seen companies in digital health struggle to get paid for their services because they must demonstrate their value to obtain a contract, yet, they need a contract to be able to truly demonstrate their outcomes in a sustainable way. The model Dreem uses works well, but it relies on existing CPT codes to cover a significant portion of the service model.”
Likewise, Omada Health has successfully navigated the fee-for-service reimbursement landscape, even working with the American Medical Association to create an entirely new CPT code specifically for the online delivery of their Diabetes Prevention Program. Omada’s Chief Privacy & Regulatory Officer, Lucia Savage, is a leading advocate for the future of the V1C industry, noting that there are many opportunities to continue to evolve the reimbursement landscape to better align with V1C delivery models.
“Reimbursement structures should focus on how we safely achieve desired member outcomes rather than quantifying interactions or limiting where providers deploy their expertise. High-quality healthcare can occur in modalities that do not have physical locations or fit within time-based structures.”
Check out the payment vignettes in the toolkit for more information on Omada and Dreem’s delivery models and reimbursement strategies.
Shaping the future of healthcare
V1C providers develop patient-centric solutions that increase access to affordable primary and specialty care services by addressing historical barriers including access, cost, and equity. The sustainability of these innovative models is critical to expanding affordable access to high-quality healthcare.
Identifying the appropriate coding and reimbursement strategies will allow these organizations to achieve financial sustainability to continue to deliver holistic care while generating the clinical and economic evidence required to develop more innovative payment models for the future.



