DIME PROJECT

Building healthcare around the patient, not the clinic

THE BLUEPRINT | SECTION 1
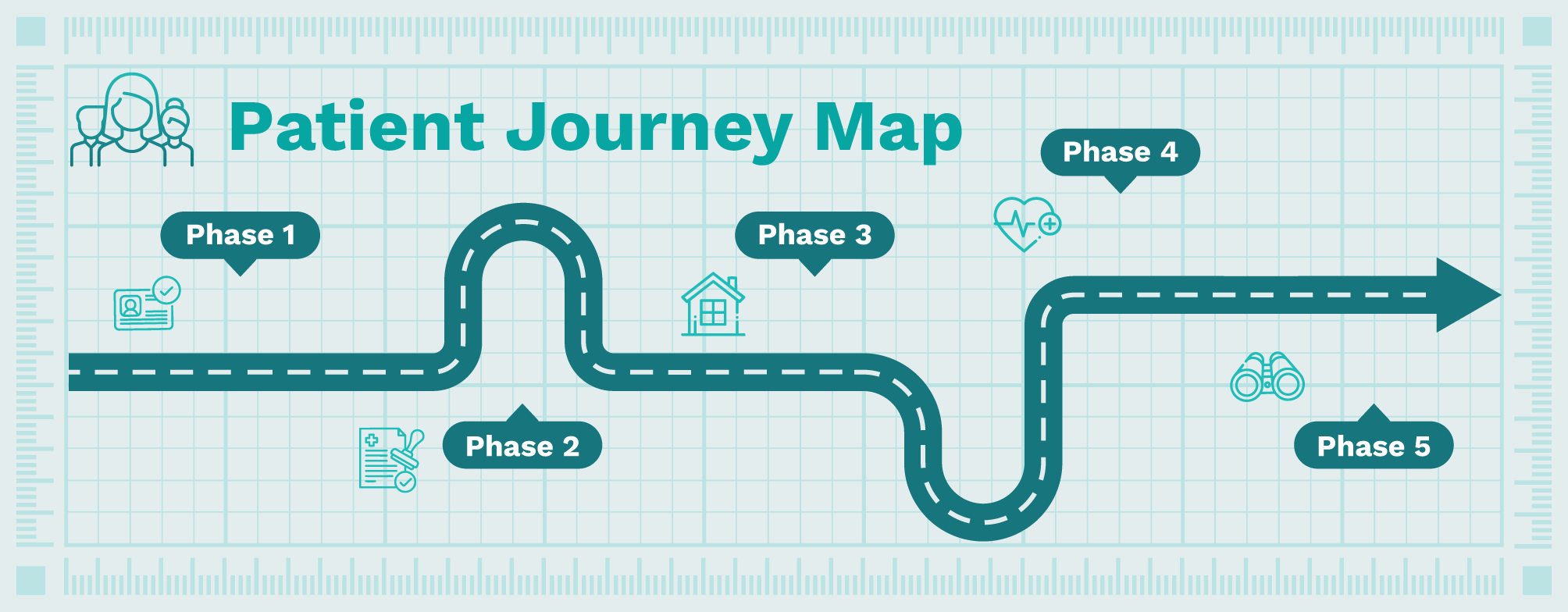
Patient Journey Map
Use the Patient Journey Map to discover all five phases of hospital-at-home (HaH)—from initial patient identification to smooth discharge and transition back to community care. Each phase includes specific action items, best practices, and critical checkpoints to help you build standardized workflows that improve patient outcomes and program sustainability. This section gives you an overview, while the next, Technical & operational considerations, dives deep into more detailed information and resources to support each phase.
 Phase 1: Identification, referral/consult, & assessment
Phase 1: Identification, referral/consult, & assessment
Patients needing acute care are considered for HaH through two main pathways:
- Continuing their acute-level care at home after inpatient admission, or
- Direct referrals/transfers from the emergency department (ED), as well as outpatient clinics, urgent care, or home, if applicable.
Once identified or referred, patients receive comprehensive assessments from the HaH intake team or their current brick-and-mortar (BAM) team, covering both clinical appropriateness and social factors. Assessments are completed through the electronic health record (EHR), video, telephone, or in-person. The patient’s final eligibility determination integrates assessment with risk stratification, including the patient’s functional status and their social determinants of health (SDOH), before it is documented and the recommendation is communicated to the patient and their care partner.

- Identify patients and utilize referrals facilitated by checkpoints, rules-based logic, and artificial intelligence (AI) to flag eligibility based on factors such as age, chief complaint, diagnosis, payor type, ZIP code, and current medication.
- Review all identified patients before referral to confirm appropriateness and minimize false positives.
- Standardize referral workflows using structured EHR forms that capture required clinical, social, and logistical data.
- Educate referring providers on eligibility criteria, referral timing, and how to introduce HaH to patients.
- Train intake staff to identify incomplete or inaccurate referrals and initiate follow-up when needed.

- Apply program-specific eligibility criteria to referred patients, ensuring timely triage of appropriate referrals to the clinical team, avoiding delays in care transition.
- Perform clinical and social assessments using standardized tools as well as patient and care partner input.
- Conduct a comprehensive clinical evaluation to confirm diagnosis, acuity, and medical stability for hospital-level care at home, specifically an in-person history and physical (H&P) exam by a HaH or BAM provider, if not scheduling for home.

- Use structured risk stratification tools to proactively flag patient-specific needs and safety concerns that may affect care delivery (e.g., cognitive status, language, complex medication regimens, care partner support, transportation, broadband access).
- Finalize eligibility based on combined clinical and social assessments.
- Clearly document the eligibility decision and communicate next steps to the patient and care partner.
 Phase 2: Consent & planning
Phase 2: Consent & planning
After confirming eligibility, a more detailed overview of the HaH program will be shared with the patient, explaining the roles and responsibilities of all stakeholders involved in their care. This includes the patient, care partner, and the multidisciplinary HaH care team. Following this explanation and addressing questions, informed consent to participate is obtained. The patient’s initial care plan is developed with admission orders guided by standard order sets. Arrangements are made to deliver necessary technology, such as digital health technologies (DHTs) for remote patient monitoring (RPM) and telehealth, and any required durable medical equipment (DME), to the patient’s home. The final planning steps coordinate practical details for the transition, including arranging transportation if needed, ensuring initial medications are delivered, and scheduling the first in-home appointments with the HaH team.

- Provide a clear, plain-language overview of the HaH model, including the scope of services, care team roles, and use of in-home technology.
- Use supplemental resources (e.g., videos, handouts) to support learning and address patient and care partner questions.
- Introduce the multidisciplinary care team, including physicians, advanced practice providers (APPs), registered nurses (RNs), rehabilitation therapists, Mobile Integrated Health (MIH) paramedics, pharmacists, case managers, and social workers, and explain each role in the HaH model.
- Obtain formal informed consent using standardized documentation, ensuring patients acknowledge responsibilities, care expectations, and escalation pathways.

- Initiate the patient’s admission using standardized order sets and HaH program protocols, including orders written during an initial history and physical (H&P) exam (if already performed) or developed at this stage based on available clinical information.
- Develop or review the initial plan of care, including working diagnosis, treatment goals, visit frequency, and assigned care team members.
- Confirm that documentation aligns with regulatory standards for the timing and content of the in-person or virtual exam.
- Initiate outcomes tracking, collecting baseline data upon admission, and establishing the care episode for monitoring.

- Select and order appropriate DHTs, such as RPM technologies and telehealth platforms, based on clinical need, regulatory status, usability, and data capture requirements.
- Ensure that all technology is compatible with the patient’s and care partner’s capabilities, taking into account broadband access and health literacy.
- Order required DME and medical supplies, confirming availability, delivery coordination, and in-home setup requirements.
- Track all technology and equipment assets for future retrieval and inventory management.

- Coordinate non-ambulance transport home when needed, recognizing transportation is a common bottleneck and source of delays.
- Arrange for the timely delivery of initial medications and ensure alignment with the care plan and prescribing protocols.
- Schedule the first in-home visits across RN/MIH, provider, and ancillary team members to ensure a seamless initiation of care.
- Schedule the in-person H&P exam to occur promptly after arrival home if not yet completed by a HaH or BAM provider.
- Communicate all logistics clearly to the patient and care partner, including expected timing and contact information for support.
-
 Phase 3: Preparation & initiation
Phase 3: Preparation & initiation
Once home, the patient’s HaH care begins with the initial in-home clinical visit, which includes a comprehensive physical assessment, checking vital signs, reviewing medications, and performing necessary interventions based on the plan of care. A critical step in ensuring patient safety is evaluating the patient’s home environment, using a safety checklist to ensure adequate space for medical equipment and clear emergency access. The required DHTs for remote monitoring and telehealth are installed, with the team confirming equipment connectivity, providing training for use and self-monitoring, and explaining how to access tech support for troubleshooting. The patient’s first at-home consultation with the HaH provider then takes place to review the plan of care and verify medical orders, which may occur in-person or virtually via telehealth, depending on prior assessments.

- Conduct a comprehensive at-home clinical assessment upon arrival, including medication reconciliation, wound or condition-specific checks, and initial interventions.
- Collect and document vital signs at least twice daily or based on program requirements.
- Confirm the patient and care partner are aware of the plan of care and what to expect from upcoming visits.
- Identify any immediate clinical, logistical, or safety concerns that require escalation or provider input.

- Complete a standardized home safety checklist to evaluate space for medical equipment, lighting, falls risk, utilities, and emergency egress.
- Ensure the home environment is stable and accessible for staff, equipment, and urgent care in the event of an escalation.
- Identify any barriers (e.g., pets, mobility hazards, clutter) that could affect care delivery or patient safety.
- Document any modifications or supports needed and communicate them to the care team promptly.

- Install DHTs such as RPM and telehealth tools, and confirm connectivity.
- Provide clear, hands-on instruction to the patient and care partner on how to use each DHT, including daily routines for self-monitoring.
- Walk through basic troubleshooting steps and explain how to reach technical support if issues arise.
- Confirm that data is transmitting correctly to the care team dashboard and is linked to the patient’s record.

- Conduct the provider’s first at-home consultation, either in-person or via telehealth, based on whether the history and physical (H&P) exam was completed prior to the patient’s transition home.
- Review the established plan of care with the patient and their care partner, addressing any questions and confirming knowledge transfer.
- Verify, adjust, or add to clinical orders based on current assessment and patient feedback.
- Set expectations for ongoing visits, monitoring, communication, and what to do in the event of a concern or emergency.
 Phase 4: Care delivery & monitoring
Phase 4: Care delivery & monitoring
Throughout their HaH episode of care, patients have scheduled clinical appointments, including regular in-person clinical visits and virtual telehealth rounds with providers. RPM collects vital signs and data is reviewed between visits by the HaH care team, with automated alerts and clinical decision support systems (CDSS) assisting with triage and decision-making. Care team coordination facilitates responsive care through daily rounds and shared documentation access, allowing for prompt responses and activating escalation pathways as needed. Ongoing resource management coordinates pharmacy services like medication refills, medical supplies and DME, mobile labs and imaging, and connects patients with community partners and support.

- Conduct in-person visits by RNs, MIH paramedics, rehabilitation therapists, phlebotomists, home health aides, and others as outlined in the care plan.
- Schedule virtual or in-person visits from physicians or APPs to monitor progress.
- Adjust visit frequency based on changes in acuity, clinical need, or patient preference.
- Ensure all team members document interactions consistently in a shared record to support coordinated care.
- Conduct video visits by RNs/MIH paramedics for witnessed medication administration, as appropriate.

- Collect and review remote vital signs and symptom data, continuously or on-demand, via RPM to complement in-person monitoring.
- Ensure secure transmission of data to the HaH care team through cellular or Wi-Fi connectivity, with integration into the patient’s record.
- Use validated CDSS and automated alerts to identify changes in status requiring intervention.
- Establish clear thresholds and escalation protocols for abnormal RPM findings.

- Conduct daily team huddles or virtual rounds using shared documentation to support continuity and alignment across disciplines.
- Coordinate facility-based care for services not deliverable in the home (e.g., advanced imaging or procedures).
- Respond promptly to RPM alerts, patient or care partner concerns, and staff observations indicating a change in status.
- Activate care escalation protocols when needed, including ED transfer or direct inpatient admission.
- Maintain real-time communication channels across all care team members to ensure rapid coordination of care changes.

- Coordinate ongoing delivery of medications, DME, and wound care or lab supplies.
- Facilitate mobile diagnostics (labs, imaging) as needed for continued assessment and care at home.
- Maintain inventory and replenishment schedules for clinical equipment, technology, and disposables.
- Engage community-based organizations or support services to address non-clinical needs (e.g., food, care partner relief).
 Phase 5: Discharge planning & care transition
Phase 5: Discharge planning & care transition
The patient and care partner engage in shared decision-making with their HaH care team to determine when discharge is appropriate based on meeting clinical goals. Readiness is confirmed by a final provider assessment, which can be conducted in-person or via telehealth, resulting in formal discharge orders and a comprehensive discharge summary. For a smooth and safe transition back to community care, the HaH team coordinates with the patient’s primary care provider (PCP) and specialists, sharing necessary information and performing a final medication reconciliation. Follow-up appointments and arrangements for needed outpatient or home care services are scheduled. The patient and care partner receive final instructions covering continued self-monitoring, follow-up plans, and contacts for urgent concerns. Logistics are finalized, including scheduling the retrieval of HaH technology and equipment, and documentation for outcome tracking is completed by the care team.

- Assess clinical progress and stability through shared decision-making between the patient, care partner, and HaH care team.
- Conduct a final in-person or virtual provider assessment to confirm discharge readiness and address outstanding clinical concerns.
- Ensure discharge decisions align with the patient’s goals and anticipated ongoing needs.

- Communicate the discharge summary and clinical handoff to the patient’s PCP and any referred specialists.
- Schedule follow-up appointments or home health services required for continued care.
- Complete final medication reconciliation and confirm the patient has access to and knowledge about their prescriptions.
- Activate any needed community-based support before the transition is complete.

- Deliver clear instructions covering symptom monitoring, escalation procedures, and contact information for post-discharge support.
- If participating in a transitional 30-day episode model, clarify that the care team may remain engaged and that HaH technology and equipment may remain in the home for continued monitoring.
- Coordinate return or deactivation of technology and equipment once the transitional phase ends.
- Complete documentation for outcomes tracking, including 30-day metrics such as readmissions, ED visits, and follow-up engagement.