DIME EVENTS
We look forward to collaborating with the DiMe community at in-person and virtual events to exchange ideas and foster innovation to ignite change across the digital health ecosystem.
Sign up for our monthly newsletter today to hear about the latest DiMe event updates and other important news!

DiMe Webinar: Transforming clinical trials with sensor-based digital health technologies (sDHT)
Virtual | 11 a.m. ET
February 4, 2026
DiMe Launch: A new era for pediatric rare diseases: Adopting evidence-based digital measures to improve patient outcomes
Virtual | 11 a.m. ET
Jan 29, 2026

Hlth Masterclass: Designing Evidence that Pays: Aligning Value Between Innovators and Payers
Virtual | 11 a.m. ET
Jan 28, 2026
SCOPE Summit 2026
Orlando, FL (USA)
Feb 2 – 6, 2026
Enjoy a $200 discount with code: PO200

ViVE 2026
Los Angeles, CA (USA)
Feb 22 – 25, 2026
Enjoy a $250 discount with code: V26_DIME250


Biotech Showcase
San Francisco, CA (USA)
Jan 12 – 14, 2026
Enjoy a $200 VIP discount with code: supDIME2025
Register here


Healthcare 2030: Building Massively Better Healthcare
Virtual | 11 a.m. ET
December 2, 2025







Building the future of hospital-at-home: Strategies for sustainable, scalable care
Virtual
June 4, 2025
Food as Medicine Network: LIVE 2025
Chicago, IL
May 7 – May 8, 2025
20% Discount code: DIME20
Digital Health Nexus Conference
San Francisco, CA (USA)
May 7 – 8, 2025
DIME-20 for 20% off




Unlocking impact through investment: Building the business case for digital endpoints
Virtual
March 26, 2025


Integrated Evidence Plans: Streamlining evidence for commercial success to drive broad acceptance of Digital Health Technologies
Virtual
March 18, 2025





Breaking Barriers with Digital Health Technologies: Advancing CRS Risk Prediction
Virtual
February 13, 2025


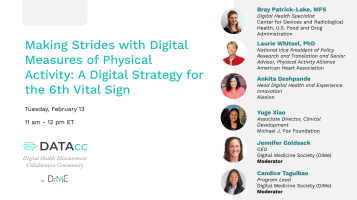
DiMe Webinar: Showcasing biotech success stories: digital endpoints in clinical trials
Virtual
January 28, 2025


Biotech Showcase
San Francisco, CA (USA)
January 13 – 15, 2025
$200 off discount code: DIME200



Insights into New Quality Benchmark for MedTech Products: An Independently Awarded Seal of Evidence, Usability, Privacy, Security & Equity
Virtual
December 12, 2024 | 12 p.m. ET
Accelerating the Path to Approval: Validating Novel Digital Clinical Measures
Virtual
December 10, 2024 | 11 a.m. ET

Scaling Digital Health Globally: Navigating National Pathways for Patient Access
Virtual
November 19, 2024 | 10 a.m. ET
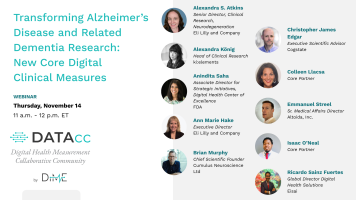
Transforming Alzheimer’s Disease and Related Dementia Research: New Core Digital Clinical Measures
Virtual
November 14, 2024 | 11 a.m. ET

Introducing the DiMe Seal: An Information Session for Developers
Virtual
Thur., Oct 31, 2024 | 11:00am ET

DiMe Journal Club: Regulatory Pathways for Qualification and Acceptance of Digital Health Technology-Derived Clinical Trial Endpoints: Considerations for Sponsors
Virtual
October 30, 2024 | 11 a.m. ET

Introducing the DiMe Seal: An Information Session for Providers, Health systems, and Payors
Virtual
Tues., Oct 29, 2024 | 11:00 am – 12:00 pm ET

World Drug Safety Congress Americas
Boston, MA (USA)
October 29-30, 2024
50% off discount code: DIME50
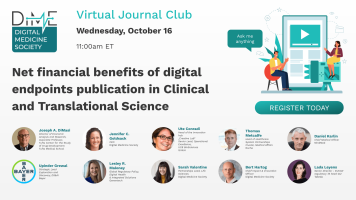
DiMe Journal Club: Net financial benefits of digital endpoints publication in Clinical and Translational Science
Virtual
October 16, 2024 | 11 a.m. ET


DiMe Journal Club: Wearable Digital Health Technology
Virtual
October 3, 2024 | 11 a.m. ET

ConV2X Telehealth Symposium entitled “Blending Health Technology to Meet Patient Needs
New York City, NY, USA
October 1-2 2024




Advancing Equity and Reducing Financial Toxicity in Cancer Care: Resources to Quantify and Maximize the Value of Digital Patient Navigation
Virtual
August 27, 2024 | 11 am ET
Public Workshop | Using Patient Generated Health Data in Medical Device Development: Case Examples of Implementation Throughout the Total Product Lifecycle
Virtual
June 26-27, 2024
Digital Measurement of Nocturnal Scratch: New Developments: Processes, Validation, and Adoption
Virtual
June 18 | 11 a.m. ET
Digital Measurement of Nocturnal Scratch: New Developments | Updates from R&D on Algorithms and Tools
Virtual
June 11 | 11 a.m. ET
Digital Measurement of Nocturnal Scratch: New Developments: Recent Regulatory Feedback
Virtual
June 4 | 11 a.m. ET


DiMe Webinar: With tightening digital health funding and escalating expectations, how can innovators efficiently construct evidence for their products?
Virtual
May 21, 2024 | 11am EST

DiMe Webinar Sleep Launch: Advancing Sleep Research: New Core Digital Measures & Resources
Virtual
April 24 | 11am ET

DiMe Webinar: Clinical trial efficiency using data and digital health tech
Virtual
April 18 | 11 am ET

Data-Driven, Hybrid, and Fully Decentralized Clinical Trials Event
Philadelphia, PA (USA)
April 16 – 17, 2024
P24DCTDIME = 15% off


Journal Club: Defining the Dimensions of Diversity to Promote Inclusion in the Digital Era of Healthcare
Virtual
March 27, 2024

V3+: An extension to the V3 framework to ensure user-centricity and scalability of sensor-based digital health technologies
Virtual
Feb 27, 2024 | 11am ET


DiMe Journal Club: The promise of artificial intelligence (AI) and machine learning (ML) for improving clinical outcomes
Virtual
February 15, 2024 | 11 am ET

SCOPE Summit 2024
Orlando, FL (USA)
Feb 11-14, 2024
For a discount use DIME ($200 off) when registering.

DiMe Journal Club: Incorporating digitally derived endpoints within clinical development programs by leveraging prior work
Virtual
January 18, 2024 | 11 am ET

J.P. Morgan 42nd Annual Healthcare Conference
San Francisco, California (USA)
Jan 8-11, 2024





