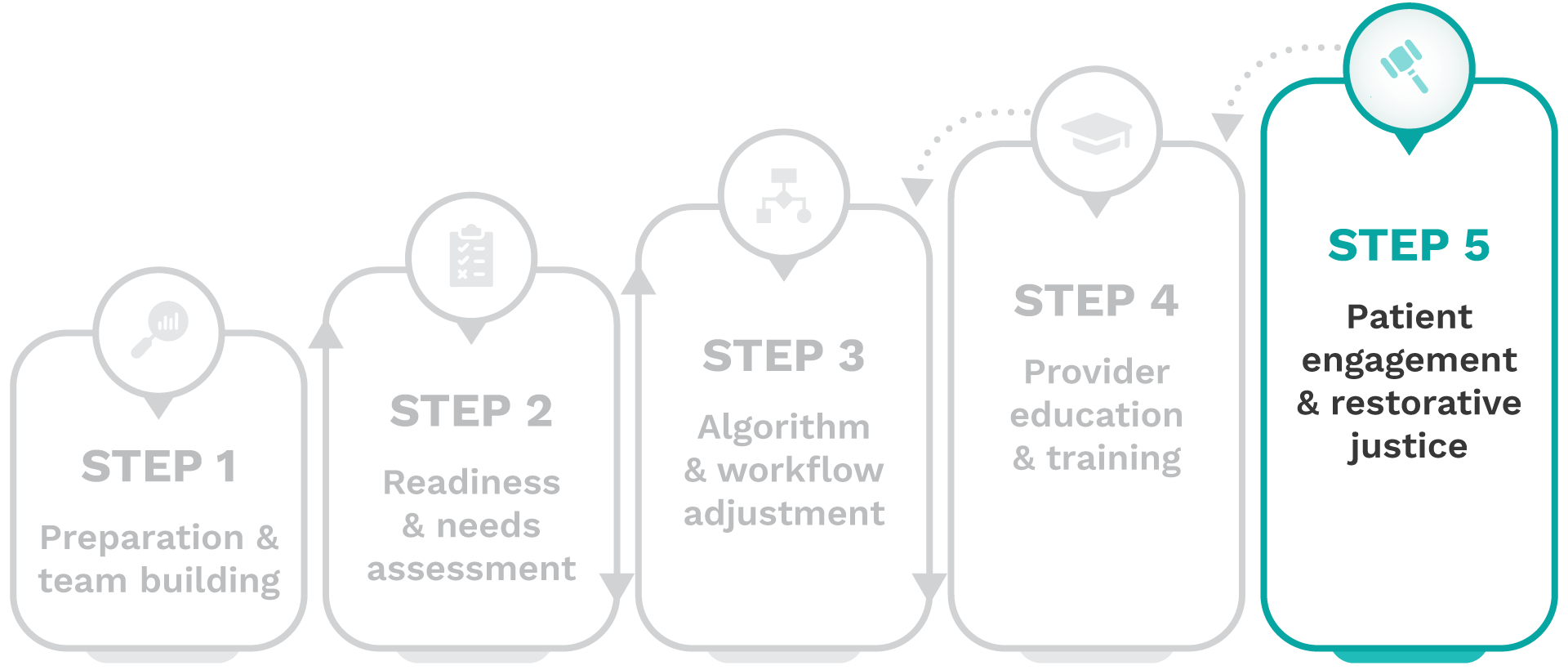
Removing harmful race-based clinical algorithms: A toolkit

Step 5-Patient engagement & restorative justice
Engaging patients in meaningful conversations about changes to their care is essential. In this step, you will learn how to address medical racism, acknowledge past harms, and foster healing through a restorative justice framework.
Important stakeholders
A multidisciplinary team that includes all staff involved in and affected by harmful algorithm de-implementation, such as executive champions, health equity leadership, clinicians and trainees, information technologists, qualitative and quantitative data scientists, and non-clinical roles like policy, operations, training, and education personnel, along with external experts and mentors including historians, social scientists, anthropologists, and patient advocacy groups.
Complete these activities
To achieve this goal, complete the following activities:
1. Commit to action and restorative justice
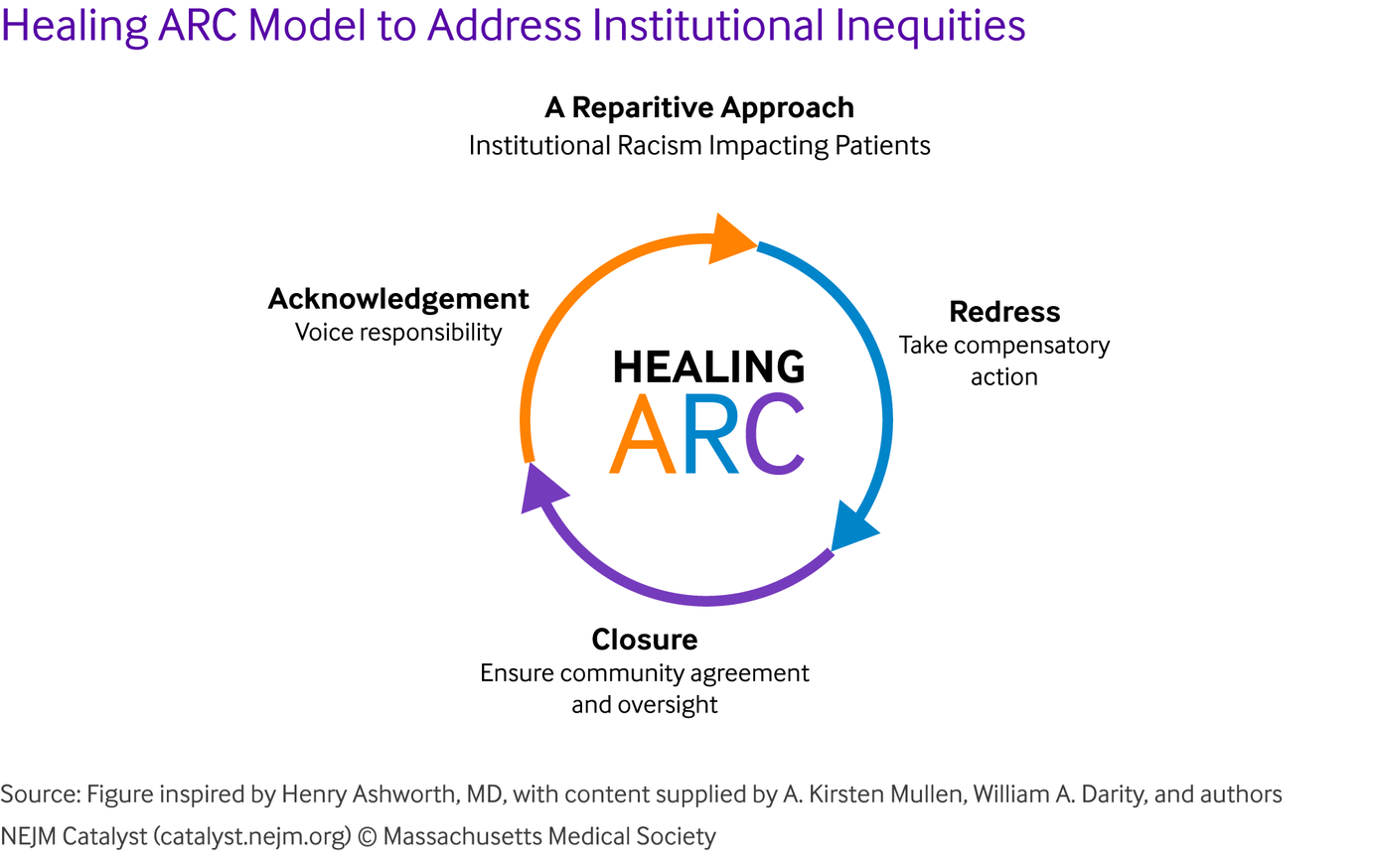
Pursuing restorative justice can be complex and may face resistance. The Healing ARC framework, a race-conscious approach utilized by CERCA, offers a structured, evidence-based approach to redressing inequities and can help guide your institution’s efforts toward meaningful action and accountability.
- Healing ARC Model to Address Institutional Inequities: Visit website
2. Pursue funding for patient engagement
Identify and pursue funding opportunities to support robust patient engagement initiatives within a restorative justice framework.
3. Facilitate patient dialogues
Facilitate open dialogues and create safe spaces for patients to share their experiences with algorithmic bias and medical racism.
4. Update your patients
Educate patients about the changes in their care as a result of de-implementation and the rationale behind the changes.
Engaging patients as true partners in healthcare decision-making can be challenging. Consider using the VBAC co-responsibility model as an example of how shared decision-making can empower patients and build trust.
- Co-responsibility in VBAC: empowering patients and clinicians for equitable birth planning: View case study
5. Provide specialty referrals
Provide referrals to specialty providers who may join the care team as a result of changes to the treatment plan.
6. Hold yourself accountable to patients
Facilitate patient-led discussions to share insights with providers, executives, and public health officials, fostering accountability and ongoing program improvements as part of a learning health system.
7. Highlight engagement opportunities
Communicate how patient feedback influenced workflow changes and care delivery while highlighting ongoing opportunities for patient involvement.
Patient engagement materials
Educational and advocacy information on Vaginal Birth After Cesarean (VBAC) for women and birthing people, families, and health care providers
CERCA
What the New Kidney Function Calculation Means for Your Kidney Disease Diagnosis and Treatment
National Kidney Foundation
Uncover how this patient’s journey with kidney disease ignited her passion for advocacy
National Kidney Foundation
Racial disparities in Chronic Kidney Disease (CKD) stem from historical inequities and social determinants of health (SDOH), not race itself
National Kidney Foundation
Clinical Outcome Measures: eGFR
PRIORITIZED TOP 5: Primary
- Referral or current care provided by nephrologist
- Referral or waitlist status for kidney transplantation
- CKD stage reclassification Utilization of
- medications to slow CKD progression
- Prevalence of CKD by stage
Clinical Outcome Measures: PFT
PRIORITIZED TOP 5: Primary
- Diagnosis of lung disease
- Referral to pulmonologists
- Prevalence of obstructive & restrictive pulmonary disease, overall & by severity
- Prescription of medications for lung diseases as recommended by COPD & asthma guidelines
- Reclassification of lung disease severity
Clinical Outcome Measures: VBAC
PRIORITIZED TOP 5: Primary
- VBAC rates
- TOLAC rates
- Postpartum complication rates
- Vaginal birth rate
- Primary and repeat cesarean rates
What’s next?
Once you have completed these activities, your patients will be empowered and engaged throughout the de-implementation process, fostering trust with their providers, transparency in their care plans, and accountability to race-conscious best practices. But the work doesn’t stop here.
De-implementation is an ongoing process—as you engage patients, you may need to revisit Steps 3 and 4 to refine workflows, strengthen provider education, and ensure lasting change. Every iteration brings you closer to a healthcare system that truly serves all patients.



