Insulin, Innovation, and Inequity
The recent failure to secure an insulin cost cap is a stark reminder that we cannot innovate first and wait to incorporate equity.
In January 1922, the first injection of insulin saved the life of a little boy called Leonard Thompson. Large-scale insulin production started almost immediately.
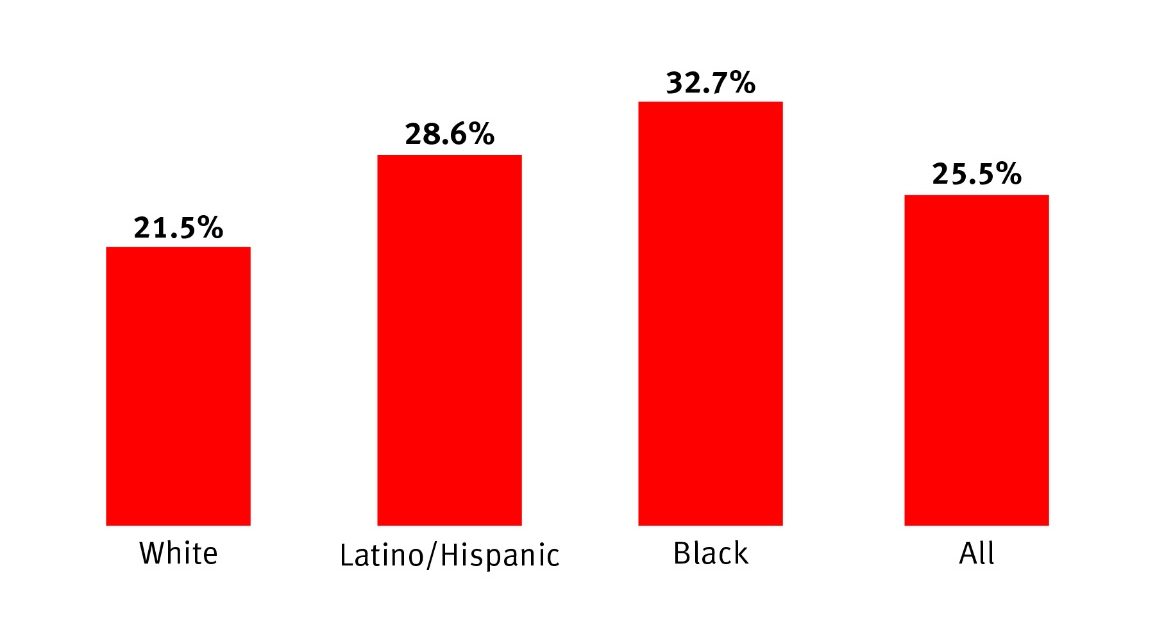
One hundred years later insulin remains the lifesaving drug for patients with diabetes. Yet one in four Americans with diabetes ration insulin due to high costs, and a Human Rights Watch report found that unaffordable insulin in the US is endangering lives. Still, lawmakers were unable to pass legislation to make this century-old innovation affordable for those who need it.
Amazon, the largest tech company in the world, has abandoned home-grown solutions in favor of buying up tech-enabled care delivery solutions while investors are pouring tens of billions of venture dollars into digital innovation. Simultaneously, healthcare decision-makers are looking to technologies like AI to offset the healthcare delivery crisis caused by the Great Resignation. In this landscape of marked transformation, we must incorporate equity in innovation.
Cost-Related Insulin Rationing Fuels Racial and Ethnic Health Disparities for People with Diabetes
Source: Herkert, Vijayakumar, Luo, et al.. Data visualized by Human Rights Watch.
Incorporating Equity into Digital Health Solutions
The digitization of healthcare presents the opportunity of our lifetime to address the most pressing challenges. Mental healthcare needs are 24/7, not Monday to Friday from 9-5. Centers of clinical excellence offer little value to patients who don’t live locally. People who could benefit most from high-touch, holistic care are least able to access it. And most of the clinical decisions made today are based on research that doesn’t reflect real-world scenarios.
However, solutions are within reach. We can use telehealth and virtual care to make the best healthcare available to anyone at any time. We can combine digital tools, analytics, and team-based care to extend the impact of clinicians. And we can use existing data, like medical records, coupled with telehealth, sensor technologies, and advanced analytics to reduce the burden of research study participation, uncovering new treatments that work for everyone.
These digital innovations, designed with intent, can absolve clinicians from the administrative burden that is impeding their capacity to care for patients and the primary driver of burnout. The use of connected technologies and the relative ease of analyzing population-level data opens the door to a system that focuses on health promotion and doesn’t require somebody to be sick before it acts.
We have the data and scientific capabilities to identify people at risk, detect the earliest signs of disease, and monitor disease burden and progression. What we are lacking is the collective will to move away from the current sick care system towards a healthcare system that cares equally well for every patient and the professionals who provide care. The incentives driving our healthcare industry and government have consistently failed to ensure equity in health and healthcare. Our industry, and those who support us with funding and policies, must insist on incorporating equity into the development and deployment of digital health solutions.
Changing Incentives to Deliver Equitable and Inclusive Digital Health Care
If we continue to reward unicorns that ease access prescriptions for erectile dysfunction, but fail to invest in digital solutions for the financial toxicity that accompanies each cancer diagnosis, we are throwing away the opportunity to reimagine healthcare in the digital era. If we favor digital innovation that provides ‘direct to consumer’ healthcare, bypassing health insurance and giving people the ‘power of the purse’ to purchase their healthcare, what future do we imagine for people whose purses are empty after the monthly bills have been paid?
Perverse Inventive and a Bloated System Keep Prices for People with Diabetes High as Drug Company Revenues Hold Steady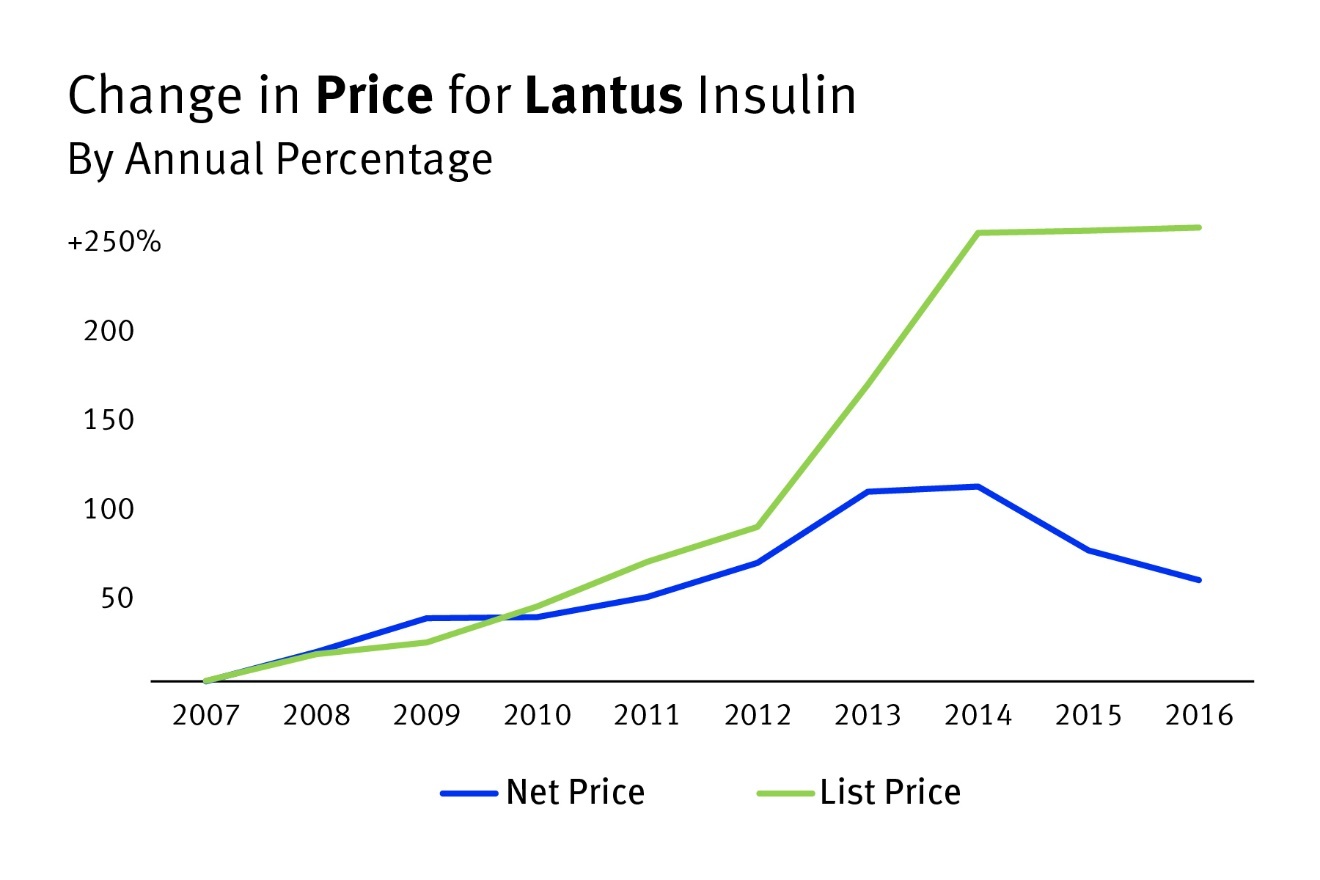
Source: Cefalu, Dawes, et al.. Visualization and commentary from Human Rights Watch.
The potential for digital health to create an affordable healthcare system that delivers good health to all has never been greater. Nor has the risk that we squander this opportunity making health disparities worse along the digital divide.
We must focus our approach to equity on health outcomes. If we make pulse oximeters available to everyone in a pandemic, but they aren’t accurate for dark skin tones, they’re not equitable. If we make tools available to everyone but don’t train people with low-tech literacy, we’re not being equitable. If we develop solutions that work in academic medical centers but aren’t helpful in rural hospitals, we’re not being equitable.
We need incentive structures that drive the transformational power of investment, innovation, and competition to harness the promise of digital innovation to address the most pressing challenges. We need policy and regulatory changes that fast-track reviews and approvals for solutions that deliver equity and inclusion. We need to demonstrate to investors that the return on investment for socially inclusive digital health innovators and products exists.
When insulin saved Leonard Thompson’s life, it offered hope to every patient diagnosed with diabetes. One hundred years later, that hope remains out of reach for far too many. In this moment of rapid transformation, our decision to prioritize equity during the digitization of healthcare will affect the lives of billions in the centuries to come. Will we choose to care for everyone or just the fortunate few?