Telemedicine is Medicine: Virtual-First Care Matters and Here’s How to Do It
Telemedicine isn’t just a video visit with your doctor. It’s your Fitbit or Smartwatch monitoring your heart rate and reporting back to another device in your home. It’s the patient portal you can visit to learn more about your health condition so you avoid searching the internet and feeling paranoid about your diagnosis. It’s the labs you can do at home and schedule FedEx to pick up. Love it or hate it, telemedicine is here to stay, and for a good reason.
It’s proven to be a handy tool for patients and clinicians caring for them. Chronic diseases are becoming more prevalent and contributing to more than 86% of healthcare costs in the United States. We’re also facing a physician shortage. 2 out of 3 clinicians want more flexible work schedules and say virtual or hybrid work best fits their lifestyle.
While the market is projected to grow to $396.76B by 2027, there continues to be much debate around regulations, reimbursement policies, and the industry’s definition of “good” telemedicine. Some progress has been made, but now is the time for us to move rapidly and focus on advancing a new care delivery model. A model that focuses on coordinated whole-person care with traditional health care partners in a digitally-enabled care system.
At the Digital Medicine Society, we refer to this new model as virtual-first care or V1C. We’ve created the tools and resources you need to integrate the V1C model now.
Put Care First in V1C Care Delivery
V1C isn’t just about taking a digital approach to care delivery. It’s about supporting the human interactions between patients and their care teams. V1C has the power to improve relationships, efficiency, and remove the care team’s administrative burden. It can also improve care transitions so patients aren’t discharged from the hospital with a ton of information only to be readmitted the next day because they forgot to take their medication.
“We need to adopt a mindset that there is no start and end point to care other than birth and death. If you have a health crisis, it’s not over when you leave the hospital. That care needs to be a continual thread that runs through somebody’s life and we can build systems that make that easier to happen.” – Corinna Cornejo, IMPACT Patient Expert
A virtual-first care model can mitigate avoidable suffering, whether it’s an interactive video, email, or text message with three simple questions for the patient’s care partner. The care team can take time to check in on patients and break down complicated guidance into steps, so it’s easier to understand, making care transitions safe and seamless for everyone involved.
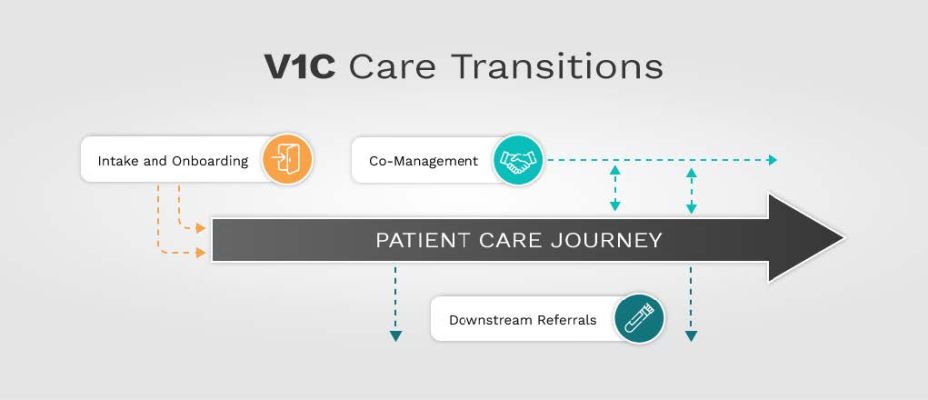
Integrate Systems for Effective V1C Care Transitions
Timely, actionable data is foundational to effective care transitions. At each phase in a patient’s care journey, access to helpful health information – in the proper format by care teams, patients, and care partners – is critical for the delivery of high-quality evidence-based care. Avoiding duplicative, conflicting care services saves time for the care team, resulting in safer patient care transitions, leading to better health outcomes.
“A huge sticking point for everyone is having these systems integrated. It doesn’t matter if the visiting nurse has an app to collect INR blood clotting for my parent, who is on a blood thinner — if that information doesn’t get to the doctor in a timely way so they can adjust the dosage, it’s not safe and effective care.” – Geri Lynn Baumblatt, IMPACT Patient Expert
By integrating and partnering with local health systems, V1C can also help solve access and clinical interoperability problems. While many great resources are available for patients, lack of access remains an issue for the medical community. Barriers to access include problems with the technology itself, the design of the information, and its cultural relevance to the patient.
Advocate for V1C Supportive Policies
Without supportive policies, new virtual care models cannot reach patients who stand to benefit the most. Seniors and people with disabilities continue to be left behind in telemedicine: blind patients cannot read results, deaf patients are not offered technology with captioning, and anyone experiencing accessibility barriers does not have energy, time, or resources to file legal complaints.
Despite these long-running inequities, broadband internet access is now recognized as a social determinant of health. In an effort to close the digital divide in the U.S., the White House has introduced the Affordable Connectivity Program (ACP), which allows tens of millions of Americans to reduce their internet service costs. This program covers more than 80% of our nation’s population across urban, suburban, and rural areas, ensuring they are offered high-speed, high-quality internet plans for no more than $30 a month.
The government’s appetite to keep and extend flexibilities for virtual-first care for our foreseeable future is strong and bipartisan. However, Medicare patients can still not receive critical chronic care services virtually, such as diabetes management and training, and in-person requirements for tele-mental health prescribers are set to resume in 2023.
More work needs to be done to overcome barriers of access, lack of awareness, and concerns over costs and integrity. Industry stakeholders can have the most impact in driving supportive policy by engaging with their local representatives, telling the stories of constituents, and presenting high-quality data that substantiate claims of improved outcomes and efficiency. We all play a role in supporting virtual-first care to better serve patients and the people who care for them.
Get Involved with our Community
You can find more examples demonstrating how V1C companies are navigating complex processes, such as payer contracting, with the help of the industry-vetted resources developed by our IMPACT collaboration.
Register today for our webinar on June 28, 2022 at 1:30 pm ET.
Hosted by the Digital Medicine Society (DiMe) and the American Telemedicine Association (ATA), vIrtual first Medical PrActice CollaboraTion (“IMPACT”) is a pre-competitive collaboration of leading digital health companies, investors, payers, and consultants dedicated to supporting virtual-first medical organizations and their commitment to patient-centric care. To become a member, visit impact.dimesociety.org to learn more and inquire about our community.
Public Launch Event: Care Transitions Supporting Effective Virtual First Care (V1C)
June 28, 2022 @ 1:30 pm ET
Join us for this 90-min launch event to learn about the overarching vision of IMPACT, meet experts from the IMPACT Steering Committee guiding its direction, and get a first look at a new suite of resources and best practices to optimize care transitions across the care continuum that will facilitate full integration of V1C into the healthcare delivery ecosystem.



