Chapter 3 – Section 3
Taking a phased approach to deployment

Taking a phased implementation approach provides a structured pathway for pediatric DHTs to evolve and adapt, incorporating user feedback and addressing emerging needs over time.
Here, you’ll learn more about the stages of DHT implementation and the actionable steps The Playbook project team recommends on how to navigate each phase successfully to optimize outcomes.
Addressing health equity with implementation science
Health equity for children demands an intentional, evidence-based approach to implementation. By structuring digital health deployment in phased steps, you can ensure that solutions are safe and accessible, and actually reach those who need them most. This approach turns intention into impact, bridging gaps in care and advancing equitable health outcomes for all children.
Phased approach
 Implement in manageable stages, allowing for adjustments based on real-world insights.
Implement in manageable stages, allowing for adjustments based on real-world insights. Adopt a flexible by design approach to meet the diverse and evolving needs of pediatric populations.
Adopt a flexible by design approach to meet the diverse and evolving needs of pediatric populations.Structured frameworks
 Enable consistent evaluation, stakeholder engagement, and alignment with children’s unique care contexts.
Enable consistent evaluation, stakeholder engagement, and alignment with children’s unique care contexts.Evidence-based deployment
 Ground decisions in data and clinical evidence to prioritize safety, effectiveness, and accessibility.
Ground decisions in data and clinical evidence to prioritize safety, effectiveness, and accessibility.
 Support equitable access to interventions across diverse settings and populations.
Support equitable access to interventions across diverse settings and populations.Performance of Routine Information System Management (PRISM):
An approach to design, strengthen and evaluate routine health information systems (RHIS). Puts emphasis on the organizational, technical and behavioural determinants of RHIS performance. Encourages and guides the development of interventions for strengthening or reforming RHIS.
Phases of DHT deployment
Explore further by hovering over the (+) sign.
Stakeholder Engagement & Needs Assessment
- Identify the needs of children, families, clinicians, and other parts of the care system.
- Engage diverse voices to ensure interventions are designed for inclusivity and relevance.
Frameworks & Evidence-Based Planning
- Use structured frameworks (like PRISM, RE-AIM) to set measurable goals.
- Prioritize user-centered, adaptable designs that address pediatric contexts.
Pilot Testing
- Implement in select, representative environments to assess feasibility and gather feedback.
- Focus on safety, usability, and accessibility for children and caregivers.
Validation of Safety & Efficacy
- Conduct controlled clinical trials or real-world testing to validate the intervention.
- Ensure the technology meets rigorous pediatric safety standards and delivers effective results.
Adaptation & Phased Scaling
- Expand implementation gradually across diverse populations and settings.
- Refine based on feedback to address barriers and support long-term engagement
Ongoing Evaluation & Improvement
- Monitor impact, adjust as children’s needs evolve, and ensure equity and quality over time.
- Focus on sustaining access and effectiveness for diverse pediatric populations.

Key insights
PRISM and RE-AIM frameworks guide inclusive practices and ensure equitable reach
When deploying pediatric DHTs, using structured frameworks, ensure an evidence-based approach that enhances the effectiveness, sustainability, and scalability of interventions. PRISM and RE-AIM can guide your development and deployment and help ensure your product is fit for users. Read more in “Applying an equity lens to assess context and implementation in public health and health services research and practice using the PRISM framework.”
Incorporate Integrated Evidence Plans
What is an IEP?
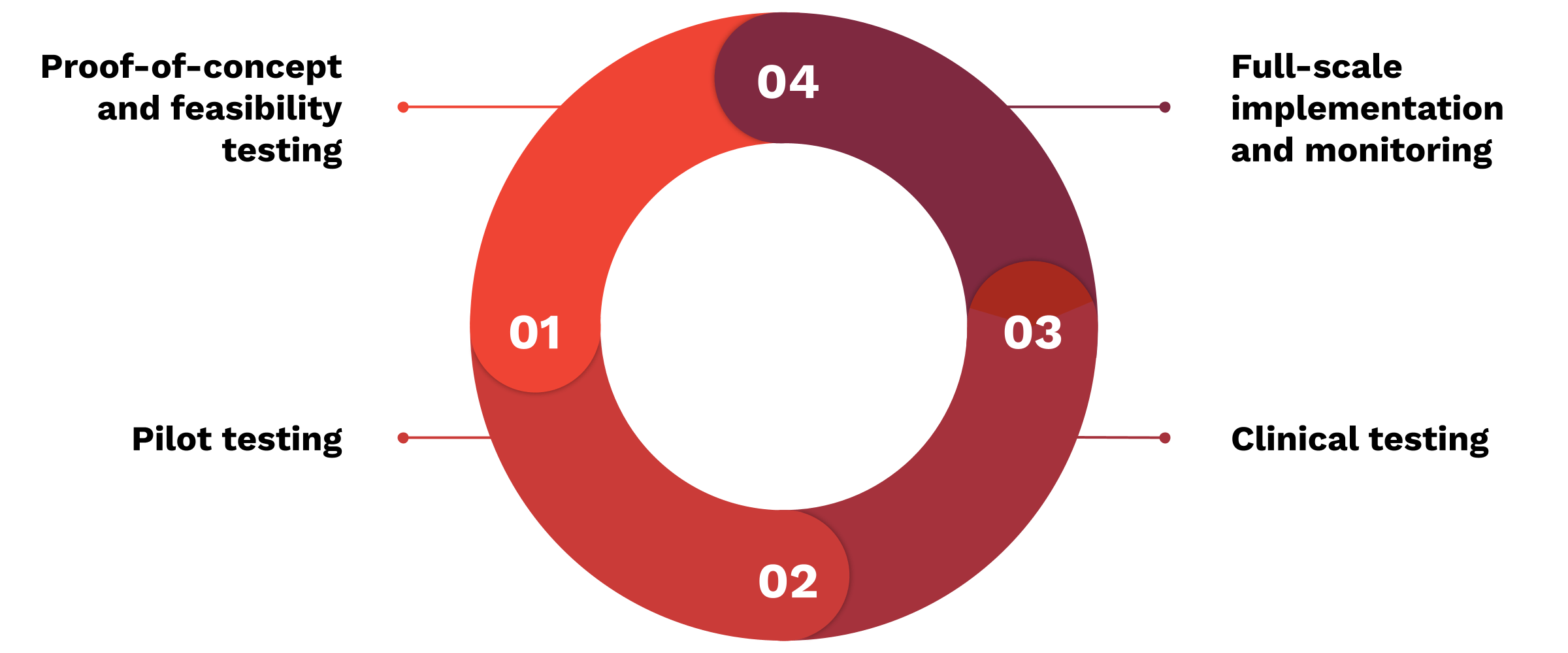
An Integrated Evidence Plan (IEP) is a strategic approach that aligns evidence generation across every phase of DHT development—proof of concept, pilot testing, clinical trials, and full-scale implementation.
Why it matters:
IEPs help ensure that digital tools for pediatric care are not only safe and effective but also developmentally appropriate and adaptable across different care settings. By incorporating consistent, age-specific data collection and feedback mechanisms, IEPs make DHTs more relevant and reliable. IEPs can streamline the collection of necessary evidence for all decision-makers on the path to market and optimize developers’ opportunities for commercial success. Learn more in DiMe’s Integrated Evidence Plan project.
Integrated Evidence Plan (IEP):
Processes and documents which outline a strategy to connect labeling concepts (i.e. the claims associated with a new drug) to the evidence-generating trials and studies in the drug program.
Scale with evidence
Develop a deliberate scaling plan early in the product life cycle, ensuring that your DHT is positioned for success in real-world environments. This process includes integrating patient- and family-centered outcome measures to demonstrate value not only to end-users, but also to payors and insurers.

- Develop a strategy early for scaling and spreading the technology from the outset of development. Collaborate with clinical partners, caregivers, and stakeholders to understand the necessary infrastructure for widespread adoption.
- Integrate family-centered outcome measures that reflect the real-world value to both families and payors. Tools should address tangible improvements in quality of life, ease of use, and healthcare costs to increase the likelihood of insurer support.
- Build an integrated evidence plan early that includes clinical validation and outcomes related to scalability and family satisfaction.
- Utilize implementation frameworks to guide your scaling strategies.
- Consider alignment with value-based care initiatives and reimbursement models that prioritize outcomes meaningful to families and insurers.
Collaborate with community networks
Community-based healthcare providers, such as pediatric-focused clinics, caregiver networks, and public health organizations, play a pivotal role in extending the reach of DHTs to underserved populations. These networks, especially in rural or low-income areas, can act as distribution hubs for DHTs, ensuring equitable access to care.

- Work with federally qualified health centers (FQHCs) to provide DHT access to Medicaid beneficiaries. Programs that integrate telehealth have been shown to improve pediatric outcomes.
- Engage local public health departments and community clinics that serve underserved communities as an avenue for patient access.
- Consider partnering with family advocacy groups such as Family Voices and Courageous Parents Network to deploy DHTs and solicit community input into your product.
Partner with pediatric systems and experts to scale DHTs
Scaling pediatric DHTs requires strong partnerships with key stakeholders, such as children’s hospitals, research institutions, and pediatric experts. These partnerships can facilitate co-development, testing, and validation of new technologies and help overcome barriers to widespread adoption.

- Collaborate with academic institutions, like children’s hospitals and research universities, to co-develop evidence-based solutions. Institutions like Boston Children’s Hospital (BCH) have pioneered innovative DHTs through partnerships with digital health developers.
- Work with well-known pediatric hospitals to develop co-branded solutions that build trust and credibility among caregivers and clinicians.
- Leverage the research capabilities of academic institutions to develop pediatric-focused studies, outcome metrics, long-term evidence-generation, and impact assessments. Consider how you might include these organizations in building an integrated evidence plan.
- Invest in pediatric-focused education initiatives to improve care delivery, especially in areas with limited pediatric services. Programs like the EMSC State Partnership Program highlight the value of child-centered medical education, and digital health tools can expand access to training resources for healthcare providers.
Case studies

Scale through schools and educational institutions
Schools represent a vital distribution channel for pediatric DHTs, particularly in addressing mental and behavioral health, chronic disease management, and preventative care. With children spending a significant portion of their day at school, integrating digital health solutions into the educational environment can create seamless care pathways and provide early intervention for health conditions. Schools also serve as key touchpoints for families and community health, offering a unique setting for scaling DHTs that reach children across socioeconomic and geographic boundaries.

- Integrate mental and behavioral health tools: Schools are critical in addressing mental health crises among children. Consider implementing screening tools and mental health management platforms within educational systems for maximum reach and benefit.
- Collaborate with educational programs: Work with state and federal education programs to secure funding and align digital health solutions with educational policies like the Every Student Succeeds Act (ESSA).
- Privacy and security in schools: Ensure robust data privacy protections, particularly under regulations like the Family Educational Rights and Privacy Act (FERPA) and the Health Insurance Portability and Accountability Act (HIPAA), when sharing health data with school-based professionals. Ensure compliance with state-specific school health mandates and data-sharing protocols when implementing DHTs in schools.
Value Based Care (VBC):
VBC focuses on patient outcomes and quality of care rather than the volume of services provided. Reimbursement is tied to the effectiveness and efficiency of care, promoting overall health and reducing healthcare costs.
Federally Qualified Health Centers (FQHCs):
Federally funded nonprofit health centers or clinics that serve medically underserved areas and populations. FQHCs provide primary care services regardless of your ability to pay. Services are provided on a sliding scale fee based on your ability to pay.